 In a few weeks the school semester will begin and many speech language pathologists will be heading back to school to resume their duties. Seasoned professionals, newly minted clinical fellows, and eager graduate students will embark on assessment and treatment of children with a variety of communication disorders. In the course of the next school year they will encounter, assess, and treat children with a number of diagnoses which result in accompanying speech language deficits. Many of these diagnoses will be familiar, a number will be new, some complex, yet others will be less known or controversial. Continue reading Introduction to the “Need to Know” Disorders in Speech Language Pathology
In a few weeks the school semester will begin and many speech language pathologists will be heading back to school to resume their duties. Seasoned professionals, newly minted clinical fellows, and eager graduate students will embark on assessment and treatment of children with a variety of communication disorders. In the course of the next school year they will encounter, assess, and treat children with a number of diagnoses which result in accompanying speech language deficits. Many of these diagnoses will be familiar, a number will be new, some complex, yet others will be less known or controversial. Continue reading Introduction to the “Need to Know” Disorders in Speech Language Pathology
Author: Tatyana Elleseff
Forms for Back to School Assessment Preparation
 Back to school time is just around the corner and if your job is anything like mine then you are getting ready to perform a number of speech language screenings and assessments after the kids get back to school in September. In order to optimize the assessment process I’ve created a number of checklists and forms for my (and your convenience). They allow for quick and efficient determination of whether the preschool/school age monolingual/bilingual student in question requires any speech language services including: screening, assessment, future follow-up, or on-going monitoring. Please note that for bilingual students it is recommended that parents mark whether the child presents with deficits in one language or in both on the checklists (e.g., mark R, E, or B – Russian, English or both).
Back to school time is just around the corner and if your job is anything like mine then you are getting ready to perform a number of speech language screenings and assessments after the kids get back to school in September. In order to optimize the assessment process I’ve created a number of checklists and forms for my (and your convenience). They allow for quick and efficient determination of whether the preschool/school age monolingual/bilingual student in question requires any speech language services including: screening, assessment, future follow-up, or on-going monitoring. Please note that for bilingual students it is recommended that parents mark whether the child presents with deficits in one language or in both on the checklists (e.g., mark R, E, or B – Russian, English or both).
- R difficulty following 3+step directions containing concepts of time or location (before/after/to the left)
- E difficulty understanding basic concepts in the classroom
- B difficulty responding appropriately to simple questions (who/what/where/when)
Speech Language Assessment Checklist For A Preschool Child is a 9 page guide created to assist speech language pathologists in the decision making process of how to select assessment instruments and prioritize assessment for preschool children 3:00-5:11 years of age. The goal is to eliminate administration of unnecessary or irrelevant tests and focus on the administration of instruments directly targeting the areas of difficulty that the child presents with.
It contains:
- Page 1 Title
- Page 2 Directions
- Pages 3-5 Checklist
- Pages 6 Suggested Speech-Language Test Selection for Preschool Children
- Page 7 Select Language Testing Battery Suggestions
- Page 8-9 Supplemental Caregiver/Teacher Data Collection Form
Checklist Target Areas:
- Receptive Language
- Memory, Attention and Sequencing
- Expressive Language
- Speech
- Voice
- Resonance
- Phonological Awareness
- Problem Solving
- Pragmatic Language
- Social Emotional Development
- Executive Functions
Speech Language Assessment Checklist For A School-Aged Child is a 12 page guide created to assist speech language pathologists in the decision making process of how to select assessment instruments and prioritize assessment for school age children. The goal is to eliminate administration of unnecessary or irrelevant tests and focus on the administration of instruments directly targeting the areas of difficulty that the child presents with.
It contains:
- Page 1 Title
- Page 2 Directions
- Pages 3-6 Checklist
- Pages 7-8 Suggested Speech-Language Test Selection for School-Aged Children
- Page 9 Select Language Testing Battery Suggestions
- Page 10-12 Supplemental Caregiver/Teacher Data Collection Form
Checklist Target Areas:
- Receptive Language
- Memory, Attention and Sequencing
- Expressive Language
- Vocabulary
- Narrative
- Speech
- Voice
- Resonance
- Phonological Awareness
- Problem Solving
- Pragmatic Language
- Social Emotional Development
- Executive Functions
Auditory Processing Deficits Checklist for School Aged Children was created to assist speech language pathologists (SLPs) with figuring out whether the student presents with auditory processing deficits which require further follow up (e.g., screening, comprehensive assessment). The SLP should provide this form to both teacher and caregiver/s to fill out to ensure that the deficit areas are consistent across all settings and people.
Checklist Categories:
- Listening Skills and Short Term Memory
- Verbal Expression
- Emergent Reading/Phonological Awareness
-
General Organizational Abilities
- Social Emotional Functioning
- Behavior
- Supplemental* Caregiver/Teacher Data Collection Form
- Select assessments sensitive to Auditory Processing Deficits
Social Pragmatic Deficits Checklist for School Aged Children was created to assist speech language pathologists (SLPs) with figuring out whether the student presents with social pragmatic language deficits which require further follow up (e.g., assessment). The SLP should provide this form to both teacher and caregiver/s to fill out to ensure that the deficit areas are consistent across all settings and people.
Checklist Categories:
- Listening/Processing
- Verbal Expression
- Problem Solving
- Pragmatic Language Skills
- Social Emotional Development
- Behavior
- Supplemental* Caregiver/Teacher Data Collection Form
- Select assessments sensitive to Social Pragmatic Deficits
You can find these products by clicking on the individual links above. You can also find many other educational products relevant to assessment and treatment in speech language pathology in my online store by clicking HERE.

Happy and successful new school year everyone!
FASD and Background History Collection: Asking the Right Questions
Note: This article was originally published in August 2013 Issue of Adoption Today Magazine (pp. 32-35).
Sometime ago, I interviewed the grandmother of an at-risk 11 year old child in kinship care, whose language abilities I have been asked to assess in order to determine whether he required speech-language therapy services. The child was attending an outpatient school program in a psychiatric hospital where I worked and his psychiatrist was significantly concerned regarding his listening comprehension abilities as well as social pragmatic skills. Continue reading FASD and Background History Collection: Asking the Right Questions
SLPs Blogging About Research: August Edition -FASD
 This month I am joining the ranks of bloggers who are blogging about research related to the field of speech pathology. Click here for more details.
This month I am joining the ranks of bloggers who are blogging about research related to the field of speech pathology. Click here for more details.
Today I will be reviewing a recently published article in The Journal of Neuroscience on the topic of brain development in children with Fetal Alcohol Spectrum Disorders (FASD), one of my areas of specialty in speech pathology.
Title: Longitudinal MRI Reveals Altered Trajectory of Brain Development during Childhood and Adolescence in Fetal Alcohol Spectrum Disorder
Purpose: Canadian researchers performed advanced MRI brain scans of 17 children with FASD between 5 and 15 years of age and compared them to the scans of 27 children without FASD. Each participant underwent 2-3 scans and each scan took place 2-4 years apart. The multiple scan component over a period of time is what made this research study so unique because no other FASD related study had done it before.
Aim of the study: To better understand how brain abnormalities evolve during key developmental periods of behavioral and cognitive progression via longitudinal examination of within-subject changes in white brain matter (Diffusion Tensor Imaging – DTI) ) in FASD during childhood and adolescence.
Subjects: Experimental subjects had a variety of FASD diagnoses which included fetal alcohol syndrome (FAS), partial FAS (pFAS), static encephalopathy alcohol exposed (SE:AE), neurobehavioral disorder alcohol exposed (NBD:AE), as well as alcohol related neurobehavioral disorder (ARND). Given the small study size the researchers combined all sub diagnoses into one FASD group for statistical analysis.
In addition to the imaging studies, FASD subjects underwent about ∼1.5 h of cognitive testing at each scan, administered by a trained research assistant. The test battery included:
- Woodcock Johnson Quantitative Concepts 18A&B (mathematics)
- Woodcock Reading Mastery Test-Revised (WRMT-R) Word ID
- Comprehensive Expressive and Receptive Vocabulary Test (CREVT)
- Working Memory Test Battery for Children (WMTB-C)
- Behavior Rating Inventory of Executive Function (BRIEF) parent form
- NEPSYI/II (auditory attention and response set; memory for names, narrative memory; arrows).
9/17 participants in the FASD group were also administered the Wide Range Intelligence Test (WRIT) at scan 2.
Control subjects were screened for psychiatric and neurological impairments. Their caregivers were also contacted retrospectively and asked to estimate in utero alcohol exposure for their child. Of the 21 control subject caregivers who were reached, 14/21 reported no exposure, 2/21 unknown, and 5/21 reported minimal alcohol exposure (range: 1–3 drinks; average of two drinks total during pregnancy). Control subjects did not undergo a full battery of cognitive testing, but were administered WRMT-R Word ID at each scan.
Summary of results: The FASD group performed significantly below the controls on most of the academic, cognitive, and executive function measures despite average IQ scores in 53% of the FASD sample. According to one of the coauthors, Sarah Treit, “longitudinal increases in raw cognitive scores (albeit without changes in age-corrected standard scores) suggest that the FASD group made cognitive gains at a typical rate with age, while still performing below average”. For those of us who work with this population these findings are very typical.
Imaging studies revealed that over time subjects in the control group presented with marked increases in brain volume and white matter – growth which was lacking in subjects with FASD. Furthermore, children with FASD who demonstrated the greatest changes in white matter development (on scans) also made the greatest reading gains. Children with the most severe FASD showed the greatest diffusion changes in white matter brain wiring and less overall brain volume.
Implications: “This study suggests alcohol-induced injury with FASD isn’t static – those with FASD have altered brain development, they aren’t developing at the same rate as those without the disorder.” So not only does the brain altering damage exists in children with FASD at birth, but it also continues to negatively affect brain development through childhood and at least through adolescence.
Given these findings, it is very important for SLPs to perform detailed and comprehensive language assessments and engage in targeted treatment planning for these children in order to provide them with specialized individualized services which are based on their rate of development.
Enough with “grow out”, “grow in” and “it’s normal” or why a differential diagnosis is so important!
If someone asked me today how long I’ve been thinking about writing this post I wouldn’t hesitate and say… 3 years. I know this because that’s when I encountered my very first case of “it’s normal”. I had been in private practice for several years, when I was contacted by parents who wanted me to evaluate their 4 year old son due to concerns over his language abilities. When I first opened my office door to let them in I encountered a completely non-verbal child with significant behavioral deficits and limited communicative intent.
I have to confess, as I was conducting an extremely difficult assessment, I was very shocked by the fact that prior to seeing me, the child had not undergone any in-depth assessments with any related professionals despite presenting with pretty significant symptoms, which included: lack of meaningful interaction with toys, stereotypical behaviors (e.g., rapid flicking of his fingers in front of his eyes for extended period of time, perseverative repetitions of unintelligible sounds out of context, etc), temper tantrums, as well as complete absence of words, phrases and sentences for his age. Very tactfully I broached the subject with the parents only to find out that the parents were concerned regarding their child’s development for quite a while, only to be told by over and over again by their pediatrician that “it’s normal”. I hastily bit back my reply, before I could rudely blurt out: “in which universe?” Instead, I finished the assessment, wrote my 8 page report with extensive recommendations and referrals, and began treating the client. Luckily, since that time he had received numerous appropriate interventions from a variety of related professionals and made some nice gains. But to this day I wonder: Would his gains have been greater had his intervention was initiated at an earlier age (e.g., 2 instead of 4)?
Of course, this is by far one of the more extreme examples that I have seen during the course of my relatively short career (less than 10 years of practice) as a speech language pathologist. But I have certainly seen others.
For example, a few years ago through my hospital based job I’ve treated a child with significant unilateral facial weakness, and a host of phonation, articulation, respiration, and resonance symptoms which included: difficulty managing oral secretions, weak voice, hypernasality, dysarthric vocal quality, and a few others. Again, the parent was told by the physician that the child’s facial asymmetry and symptomology was ‘not significant’’ despite the fact that in addition to the above signs, the child also presented with significantly delayed language development, cognitive limitations and severe behavioral manifestations.
Then of course there were a few stutterers with a host of social history red flags who stuttered for a few years well into early school age, each of whose parents were told by their child’s doctor that s/he will grow out of it.

I am not even counting dozens and dozens of phone calls from concerned parents of language delayed toddlers and preschoolers whose pediatricians told them that they’ll “grow out of it” despite the fact that many of these children ended up receiving speech language services for language delays/disorders for several years afterwards.
I’ve also seen professionals without a specialization in International Adoption diagnosing recently adopted older post-institutionalized children with history of severe trauma, profound language delays, alcohol related deficits and symptoms of institutional autism as Pervasive Developmental Disorder (PDD).
But I don’t want you to think that I am singling out pediatricians in this post. The truth is that if we look closely we will find that this trend of overconfident recommendations is common to a vast majority of both medical and ancillary professionals (e.g., psychologists, occupational therapists, etc) with speech language pathologists not exempt from the above.
I’ve read a psychiatrist’s report, which diagnosed a child with Asperger’s based on a 15 minute conversation with the child, coupled with a brief physical examination (as documented in the child’s clinical record). At my urging (based on the child’s adaptive behavior, linguistic profile and rather superior social pragmatic functioning) the parents sought a second opinion with another psychiatrist, which revealed that the child wasn’t even on the spectrum but had a anxiety disorder, some of which symptoms mimicked Asperger’s (e.g., perseveration on topics of interest).
I’ve read numerous neurological and neuropsychological reports which diagnosed children with ADD based on the symptoms of inattention and impulsivity in select settings (e.g., school only) without a differential diagnosis to rule out language deficits, auditory processing deficits, medical conditions, or acquired syndromes such as Fetal Alcohol Spectrum Disorders.
I’ve reviewed occupational therapy evaluations which reported on the language abilities of children vs. fine and gross motor function and sensory integration skills.
One parent even told me that when she asked a speech language therapist (who was treating her child for articulation difficulties) regarding her 10 year old son’s “ginormous” (parent’s words not mine) overbite she was told “he’ll grow into it”. I was told that the pediatric orthodontist did not appreciate that opinion and vigorously voiced his own as he was fitting the child for braces.
So when exactly did some of us decide that a differential diagnosis doesn’t matter? I’d be very curious to know what prompts professionals, who upon seeing some ‘garden variety’ symptoms, which could have a multitude of causes (e.g., inattention, echolalia, lack of speech, etc) decide that there could be only one definitive diagnosis or who merely shrug the displayed signs and accompanying parental concerns aside, expecting both to disappear on their own volition, given the passage of time.
Is it carelessness?
Is it overconfidence in own abilities?
Is it fear of losing face in front of the parent if you don’t have a ready answer?
Is it misguided belief that the child is displaying “textbook” behavior?
Is it “jadedness” or I’ve seen it all, so I know what it is, attitude?
I can venture hundreds more guesses, but it would be merely pointless speculation. Rather I prefer to focus on the intent of this post which is to outline why a differential diagnosis is so important!
1. Differential diagnosis saves lives!
Yes, I know I am only a speech pathologist and it’s true that I have yet to hear from anyone “I need a speech pathologist stat!” After all I don’t specialize in pediatric dysphagia and treat preemies in NICU.
But imagine the following scenario. A young preschool child shows up to your office with a hoarse vocal quality and a history of behavior tantrums. No problem you think, textbook vocal nodules, I got this, case closed! But what if the child was displaying additional symptoms such as stridor, coughing and difficulty breathing when sleeping? What if a few days after you’ve initiated voice therapy or told the parent that the child is too young for it, the child was rushed into the hospital because his airway was obstructed due to a laryngeal papilloma, which almost caused the child to asphyxiate. Still feel confident in your first diagnosis? Yet some speech language therapists routinely accept children into voice therapy without first referring them for an ENT consult that involves endoscopic imaging. Some of you may scoff and tell me, common, when does thing ever happen? Wouldn’t a doctor have picked up on something like that well before a child seen an SLP? Guess what … not necessarily!

Although it may be hard to believe but an EI or school-based SLP may be the first diagnostic professional many children from at-risk backgrounds come in contact with. Obstacles to receiving appropriate early medical care and ancillary services like early intervention may include limited financial means, lack of education or information, and cultural and linguistic barriers. Bilingual, multicultural, domestically adopted and foster care children from low-income households are particularly at risk since their deficits may not be detected until they begin receiving services in EI or preschool. After all, specialized medical care and related services must be sought out and paid for, which may be very hard to do for families from low SES households if they don’t have medical insurance or are having difficulty applying for Medicaid or state health insurance.
Similarly internationally adopted children are also at significant risk of despite the fact that most are adopted by middle class, financially solvent and highly educated parents. With this particular group the barriers to early identification are pre-adoption environmental risk factors (length of institutionalization and quality of medical care in that setting), combined with limited access to information (paucity of prenatal, medical and developmental history details in the adoption records).
2. Sometimes diagnosis DOES matter!
I know, I know, a number of you will try to convince me that we need to treat the symptoms and NOT the label! But humor me for a second! Let’s say you are a medical/ancillary professional (depending whom the child get’s to see first and for what reason) who gets to assess a new preschool patient/client, let’s call him Johnny. So little 4 year old Johnny walk into your office with the following symptoms:
- aggressive /inappropriate behaviors
- odd fine and gross motor movements
- clumsiness
- blunted affect (facial expression)
- inconsistent eye contact
- speech/language deficits
- picky eater with a history of stomach issues (e.g., nausea, vomiting, belly pain)
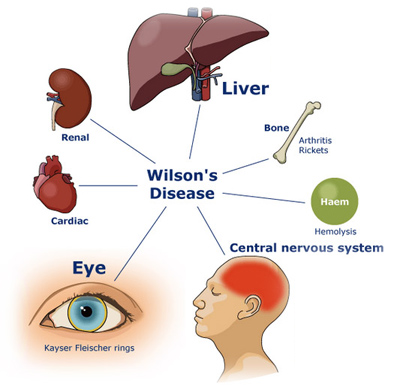
Everything you observe points to the diagnosis of Autism, after all you are the professional, and you’ve seen hundreds of such cases. It’s textbook, right? WRONG! I’ve just described to you some of the symptoms of Wilson’s disease. It’s a genetic disorder in which large amounts of copper build up in the liver and brain. This disorder has degrees of severity ranging from mild/progressive to acute/severe. It can cause brain and nervous system damage, hence the psychiatric and neuromuscular symptoms. The bad news is that this condition can be fatal if misdiagnosed/undiagnosed! The good news is that it is also VERY treatable and can be easily managed with medication, dietary changes, and of course relevant therapies (e.g, PT, OT, ST, etc)!
3. Correct Diagnosis can lead to Appropriate Treatment!
So we all know that ADHD diagnosis is currently being doled out like candy to practically every child with the symptoms of Inattention, Hyperactivity and Impulsivity. But can you actually GUESS how many children are misdiagnosed with it?
Elder (2010), found that nearly 1 million children in US are potentially misdiagnosed with ADHD simply because they are the youngest and most immature in their kindergarten class. Here’s what he has to say on the subject: “A child’s birth date relative to the eligibility cutoff … strongly influences teachers’ assessments of whether the child exhibits ADHD symptoms but is only weakly associated with similarly measured parental assessments, suggesting that many diagnoses may be driven by teachers’ perceptions of poor behavior among the youngest children in a classroom. These perceptions have long-lasting consequences: the youngest children in fifth and eighth grades are nearly twice as likely as their older classmates to regularly use stimulants prescribed to treat ADHD.” (Elder, 2010, 641)

Here are a few examples of ADHD misdiagnosis straight from my caseload.
Case A: 9 year old girl, Internationally Adopted at the age of 16 months diagnosed with ADHD based on the following symptoms:
- Inattentive
- Frequently misheard verbal messages
- Difficulty following verbal directions
- Very distractible
- Blurted things out impulsively
- Constantly forgot what had been told to her
- Made careless mistakes on school/home work
Prior to medicating the child, the parents sought a language evaluation at the advice of a private social worker. My assessment revealed a language processing disorder and a recommendation for a comprehensive APD assessment with an audiologist. Comprehensive audiological assessment revealed the diagnosis of APD with recommendations for language intervention. After language therapy with a focus on improving the child’s auditory processing skills was initiated, her symptoms improved dramatically. The recommendations for medication were scrapped.
Case B: 12 year old boy attending outpatient school in a psychiatric hospital diagnosed with ADHD and medicated unsuccessfully for it for several years based on the following symptoms:
- Severely Impulsive and Inattentive
- Occasional tantrums, opposition and aggressive behaviors
- Difficulty with transitions
- Odd Behaviors/Inappropriate Statements
- Off-topic/Unrelated Comments
- Topic Perseverations
- Poor memory
- Poor ability to follow directions
Detailed case history interview performed prior to initiation of a comprehensive language assessment revealed a history of Traumatic Brain Injury (TBI) at 18 months of age. Apparently the child was dropped on concrete floor head first by his biological father. However, no medical follow up took place at the time due to lack of household stability. The child was in and out of shelter with mother due to domestic abuse in the home perpetrated by biological father.
The child’s mother reported that he developed speech and language early without difficulties but experienced a significant skills regression around 1.5-2 years of age (hint, hint). Comprehensive language assessment revealed numerous language difficulties, many of which were in the areas of memory, comprehension as well as social pragmatic language. Following the language assessment, relevant medical referrals at the age of 12 substantiated the diagnosis of TBI (better late than never). So no wonder the medication had no effect!
So what can parents do to ensure that their child is being diagnosed appropriately and receives the best possible services from various health professionals?
For starters, make sure to carefully describe all the symptoms that your child presents with (write them down to keep track of them if necessary). It is important to understand that many conditions are dynamic in nature and may change symptoms over time. For example, children with alcohol related disorders may display feeding deficits as infants, delayed developmental milestones as toddlers, good conversational abilities but poor social behavior and abstract thinking skills as school aged children and low academic achievement as adolescents.
Ensure that the professional spends adequate period of time with the child prior to generating a report or rendering a diagnosis. We’ve all been in situations when reports/diagnoses were generated based on a 15 minute cursory visit, which did not involve any follow up testing or when the report was generated based on parental interview vs. actual face to face contact and interaction with the child. THIS IS NOT HOW IT’S SUPPOSED TO WORK! THIS IS HOW MISDIAGNOSES HAPPEN!
Don’t be afraid to ask follow up questions or request rationale for the professionals’ decisions. If you don’t understand something or are skeptical of the results, don’t be afraid to question the findings in a professional way. If the information provided to you seems inadequate or poorly justified consider getting a second opinion with another professional.
Make sure that your child is being treated as a unique individual and not as a textbook subject. Don’t you just hate it when you are trying to describe something to a professional and they look like they are listening but in reality they are not really ‘hearing’ you because they already “know what you have”. Or they are looking at your child but they are not really seeing him/her, because he/she is just another ‘textbook case’ in a long cue of clients. THIS IS NOT THE TREATMENT YOU ARE SUPPOSED TO GET FROM PROFESSIONALS! If this is how your child being treated then maybe it’s time to switch providers!
And another thing there are NO textbook clients! All clients are unique! I currently have about 10 post institutionalized Internationally Adopted children on my caseload with similar deficits but completely different symptom presentation, degrees of severely, as well as overall functioning. Even though some are around the same age, they are so dramatically different from one another that I need to use completely different approaches when I am planning their respective interventions.

Here’s how we as health professionals can better serve our clients/patients needs
It’s all in the details! Carefully collect the client’s background history without leaving anything out. No piece of information is too small/inconsequential! You never know what might be relevant.
Get down to the nitty gritty by asking specific questions. If you ask general questions you’ll get general responses. For example, numerous health care professionals in various fields (doctors, psychiatrists, psychologists, SLPs, etc) routinely ask biological, adoptive and foster parents and adoptive caregivers whether substance abuse of drugs/alcohol took place before and during pregnancy (that they know of with respect to the latter two). A number will respond that yes it took place during pregnancy but stopped as soon as the mother found out she was pregnant. Many professionals will leave it at that and move on to the next line of questioning. However, the follow up question to the above response should always be: “How many months along was the biological mother when she found out she was pregnant?” You’d be surprised at the responses you’ll get, which may significantly clarify the “mystery” of the child’s current symptomology.
Pretend that each new case is your very first case! Remember how you were fresh out of grad school/residency? How much enthusiasm, time, and effort you’ve put in leaving no stone unturned to diagnose your clients? That’s the passion and dedication the parents are looking for.
It’s always fun to play a detective! How cool was “House” when it first came out? House and his team left no stone unturned in trying to correctly diagnose their patients. At times they even went to their houses or places of work in order to find any shred of information that would lead them on the right path. Admittedly you don’t have to go quite that far, but a consultation with a related professional might do the trick if a client is exhibiting certain symptoms outside your experience.

Turn your weakness into strength! No one likes to admit that they don’t have the answer. Many of us worry that our clients (those who work with adults) or their parents (those who work with children) may lose confidence in us and go elsewhere for services. But everything depends on how you frame it! If you simply explain to the parent the rationale for the referral and why you want them to see another specialist prior to formulating the final diagnosis, they will only THANK YOU! It will show them that rather than making a casual decision, you want to make the best decision in their child’s case and they will only appreciate your candor as to them it shows your commitment to the care of their child.
It doesn’t matter how well educated and well trained many medical and related professionals are, the fact remains – no one knows everything! That is why each of us has our own unique scope of practice! That is why we should operate within our scope of practice and referral clients for additional assessments when needed. Differential diagnosis should not be an exception; it should be a rule for any patient who does not show ‘unique’ symptoms indicative of very specific disorders/conditions! It should be performed with far greater frequency than it is done right now by medical and related health professionals!
After all: “When you have excluded all possibilities, then what remains -however improbable – must be the truth”. ~Sherlock Holmes
References:
- Elder, T (2010). The Importance of Relative Standards in ADHD Diagnoses: Evidence Based on a Child’s Date of Birth, Journal of Health Economics, 29(5): 641-656.
- Zacharisen, M & Conley, S (2006) Recurrent Respiratory Papillomatosis in Children: Masquerader of Common Respiratory Diseases. Pediatrics 118 (5): 1925-1931.
- Gow P, Smallwood R, Angus P, Smith A, Wall A, Sewell R. (2000) Diagnosis of Wilson’s disease: an experience over three decades. GUT: International Journal of Gastroenterology and Hepatology, 46: 415–419.
Trivia Night Answers and Winners
Thank you all who participated in yesterday’s Trivia Night!
Below you’ll find answers to round’s questions as well as the names of winners for each round.
Round 1: Early Child Development
1. Name at least 3 characteristics of child directed speech
These include: motherese, repetition, modeling speech, simple syntax, slowing rate, using a higher pitch as well as using an exaggerated intonation pattern.
2. What is the critical period hypothesis? It is a time period during which language acquisition takes place
3. Name at least 3 functions of communicative behavior during infancy
These include: obtaining attention, seeking approval, seeking assistance, seeking attachment just to name a few
4. Name 2 types of echolalia: Immediate and Delayed
5. What is jargon and up until what age is it appropriate in children? Jargon is not true speech but rather pre-linguistic “nonsensical” vocalizations which involve adult-like stress and intonation patterns. Jargon usually begins to occur around 10-11 months of age in children and can typically last up until about 18 months of age give or take depending on the individual development rate of the child in question.
Round 2: Internationally Adopted Children
1. As related to internationally adopted (IA) children, what does the acronym CLM stand for and what does it mean?
CLM stands for Cognitive Language Mastery. It is the language needed for formal academic learning. This includes listening, speaking, reading, and writing about subject area content material including analyzing, synthesizing, judging and evaluating presented information. This level of language learning is essential for a child to succeed in school. CLM typically takes years and years to master, especially because, IA children did not have the same foundation of knowledge and stimulation as bilingual children in their birth countries.
2. ”The pattern of language acquisition in internationally adopted children is often referred to as a second first language acquisition” (Scott et al., 2011). Why? Because the first language (which is typically delayed and limited to begin with due to adverse effects of institutionalization) becomes completely obsolete as English is learned. So they end up learning L2 literally from scratch.
3. Why CAN’T we treat Internationally Adopted children as bilingual speakers? Because they are typically adopted by parents who do not speak their birth language as a result of which they experience rapid birth language attrition and forget their birth language very rapidly.
4. IA children may present with “normal” language abilities but still display significant difficulties in this area of functioning cognitive-academic and or social pragmatic communication (acceptable responses).
5. Finish the following sentence: “Any child with a known history of speech and language delays in the sending country should be considered to have true delays or disorders and should receive speech and language services after adoption.” (Glennen, 2009, p.52)
Round 3: Fetal Alcohol Spectrum Disorders
1. FASD is an umbrella term for the range of effects that can occur due to maternal alcohol consumption during pregnancy which may create physical, cognitive, behavioral, as well as learning/language deficits. It is NOT a clinical diagnosis. Please list at least 3 CURRENT terms under the FASD umbrella (see http://depts.washington.edu/fasdpn/htmls/fasd-fas.htm for details)
- Fetal Alcohol Syndrome (FAS)
- Partial FAS
- Static Encephalopathy (alcohol exposed)
- Neurobehavioral Disorder (alcohol exposed)
2. Name at least 3 characteristics of infants/toddlers with alcohol related deficits
- May show failure to thrive
- Increased sensitivity to sensory stimuli
-
Delayed speech/language milestones
-
Decreased muscle tone and poor muscle coordination
-
Poor self regulation
3. Since behavioral problems become more pronounced during the school years, many researchers found that the primary deficit of school aged children with FASD is in the area of (acceptable responses below)
- Daily Functioning Skills
- Self-regulation difficulties
- Problem Solving Issues
- Social/emotional problems
4. Finish the following sentence: adolescents with FASD have significant DIFFICULTY LEARNING FROM Experience
5. Why is early detection of alcohol related deficits important? Because it can lead to
- Early and Appropriate Service Delivery
- Improved Adaptability
- Improved Functioning
- Improved Outcomes
AND NOW THE WINNERS:
SLP Trivia Night: Round Three
1. FASD is an umbrella term for the range of effects that can occur due to maternal alcohol consumption during pregnancy which may create physical, cognitive, behavioral, as well as learning/language deficits. It is NOT a clinical diagnosis. Please list at least 3 CURRENT terms under the FASD umbrella.
2. Name at least 3 characteristics of infants/toddlers with alcohol related deficits.
3. Since behavioral problems become more pronounced during the school years, many researchers found that the primary deficit of school aged children with FASD is in the area of ____________
4. Finish the following sentence: adolescents with FASD have significant DIFFICULTY LEARNING FROM _______
5. Why is early detection of alcohol related deficits important?
Place your responses under this blog post and number each response for clarity.
The first person to get all answers correct will have their choice of product from my online store.
SLP Trivia Night: Round Two
1. As related to internationally adopted (IA) children, what does the acronym CLM stand for and what does it mean?
2. “The pattern of language acquisition in internationally adopted children is often referred to as a second first language acquisition” (Scott et al., 2011). Why?
3. Why CAN’T we treat Internationally Adopted children as bilingual speakers?
4. IA children may present with “normal” language abilities but still display significant difficulties in this area of functioning ___________.
5. Finish the following sentence: “Any child with a known history of speech and language delays in the sending country should _____________________”.
Place your responses under this blog post and number each response for clarity.
The first person to get all answers correct will have their choice of product from my online store.
SLP Trivia Night: Round One
1. Name at least 3 characteristics of child directed speech
2. What is the critical period hypothesis?
3. Name at least 3 functions of communicative behavior during infancy
4. Name 2 types of echolalia
5. What is jargon and up until what age is it appropriate in children?
Place your responses under this blog post and number each response for clarity.
The first person to get all answers correct will have their choice of product from my online store.
Dear Neurodevelopmental Pediatrician: Please Don’t Do That!
 Recently I got yet another one of the dreaded phone calls which went a little something like this:
Recently I got yet another one of the dreaded phone calls which went a little something like this:
Parent: Hi, I am looking for a speech therapist for my son, who uses PROMPT to treat Childhood Apraxia of Speech (CAS). Are you PROMPT certified?
Me: I am PROMPT trained and I do treat motor speech disorders but perhaps you can first tell me a little bit about your child? What is his age? What type of speech difficulties does he have? Who diagnosed him and recommended the treatment.
Parent: He is turning 3. He was diagnosed by a neurodevelopmental pediatrician a few weeks ago. She recommended speech therapy 4 times a week for 30 minutes sessions, using PROMPT.
Me: And what did the speech therapy evaluation reveal?
Parent: We did not do a speech therapy evaluation yet.
Sadly I get these type of phone calls at least once a month. Frantic parents of toddlers aged 18 months to 3+ years of age call to inquire regarding the availability of PROMPT therapy based exclusively on the diagnosis of the neurodevelopmental pediatrician. In all cases I am told that the neurodevelopmental pediatrician specified speech language diagnosis, method of treatment, and therapy frequency, ALBEIT in a complete absence of a comprehensive speech language evaluation and/or past speech language therapy treatments.
The conversation that follows is often an uncomfortable one. I listen to the parental description of the child’s presenting symptoms and explain to the parents that a comprehensive speech language assessment by a certified speech language pathologist is needed prior to initiation of any therapy services. I also explain to the parents that depending on the child’s age and the assessment findings CAS may or may not be substantiated since there are a number of speech sound disorders which may have symptoms similar to CAS.
Following my ‘spiel’, the parents typically react in a number of ways. Some get offended that I dared to question the judgement of a highly qualified medical professional. Others hurriedly thank me for my time and resoundingly hang up the phone. Yet a number of parents will stay on the line, actually listen to what I have to say and ask me detailed questions. Some of them will even become clients and have their children undergo a speech language evaluation. Still a number of them will find out that their child never even had CAS! Past misdiagnoses ranged from ASD (CAS was mistaken due to the presence of imprecise speech and excessive jargon related utterances) to severe phonological disorder to dysarthria secondary to CP. Thus, prior to performing a detailed speech language evaluation on the child I had no way of knowing whether the child truly presented with CAS symptoms.
Before I continue I’d like to provide a rudimentary definition of CAS. Since its identification years ago it has been argued whether CAS is linguistic or motoric in nature with the latest consensus being that CAS is a disorder which disrupts speech motor control and creates difficulty with volitional, intelligible speech production. Latest research also shows that in addition to having difficulty forming words and sentences at the speech level, children with CAS also experience difficulty in the areas of receptive and expressive language, in other words, “pure” apraxia of speech is rare (Hammer, 2007).

This condition NEEDS to be diagnosed by a speech language pathologist! Not only that, due to the disorder’s complexity it is strongly recommended that if parents suspect CAS they should take their child for an assessment with an SLP specializing in assessment and treatment of motor speech disorders. Here’s why.
- CAS has a number of overlapping symptoms with other speech sound disorders (e.g., severe phonological disorder, dysarthria, etc).
- Symptoms which may initially appear as CAS may change during the course of intervention by the time the child is older (e.g., 3 years of age) which is why diagnosing toddlers under 3 years of age is very problematic and the use of “suspected” or “working” diagnosis is recommended (Davis & Velleman, 2000) in order to avoid misdiagnosis
- Diagnosis of CAS is also problematic due to the fact that there are no valid or reliable standardized assessments sensitive to CAS (McCauley & Strand, 2008). However, a new instrument Dynamic Evaluation of Motor Speech Skill (DEMSS) (Strand et al, 2013) is showing promise with respect to differential diagnosis of severe speech impairments in children
- Thus for children with less severe impairments SLPs need to design tasks to assess the child’s:
- Automatic vs. volitional control
- Simple vs. complex speech
- Consistency of productions on repetitions of same word
- Vowel productions
- Imitation abilities
- Prosody
- Phonetic inventory BEFORE and AFTER intervention
- Types and levels of cueing the child is presently stimulable to
- in order to determine where the breakdown is taking place (Caspari, 2012)
These are just some of the reasons why specialization in CAS is needed and why it is IMPOSSIBLE to make a reliable CAS diagnosis by simply observing the child for a length of time, from a brief physical exam, and from extensive parental interviews (e.g., a typical neurodevelopmental appointment).
In fact, leading CAS experts state that you DON’t need a neurologist in order to confirm the CAS diagnosis (Hammer, 2007).
Furthermore, “NO SINGLE PROGRAM WORKS FOR ALL CHILDREN WITH APRAXIA!!” (Hammer, 2007). Hence SLPs NEED to individualize not only their approach with each child but also switch approaches with the same child when needed it in order to continue making therapy gains. Given the above the PROMPT approach may not even be applicable to some children.
It goes without saying that MANY developmental pediatricians will NOT do this!
But for those who do, I implore you – if you observe that a young child is having difficulty producing speech, please refer the child for a speech language assessment first. Please specify to the parents your concerns (e.g., restricted sound repertoire for the child’s age, difficulty sequencing sounds to make words, etc) BUT NOT the diagnosis, therapy frequency, as well as therapy approaches. Allow the assessing speech language pathologist to make these recommendations in order to ensure that the child receives the best possible targeted intervention for his/her disorder.
For more information please visit the Childhood Apraxia of Speech Association of North America (CASANA) website or visit the ASHA website to find a professional specializing in the diagnosis and treatment of CAS near you.
References:
- Caspari, S (2012) Beyond Picture Cards! Practical Assessment and Treatment Methods for Children with Apraxia of Speech. Session presented for New Jersey Speech Language Hearing Association Convention, Long Branch, NJ
- Davis, B., & Velleman, S. L. (2000). Differential diagnosis and treatment of developmental apraxia of speech in infants and toddlers. Infant-Toddler Intervention: The Transdisciplinary Journal, 10, 177–192.
- Hammer, D (2007) Childhood Apraxia of Speech: Evaluation and Therapy Challenges. Retrieved from http://www.maxshouse.com.au/documents/CAS%20conference%20day%201%20.ppt.
- McCauley RJ, Strand EA. (2008). A Review of Standardized Tests of Nonverbal Oral and Speech Motor Performance in Children. American Journal of Speech-Language Pathology, 17,81-91.
- Strand, E, McCauley, R, Weigand, S, Stoeckel, R & Baas, B (2013) A Motor Speech Assessment for Children with Severe Speech Disorders: Reliability and Validity Evidence. Journal of Speech Language and Hearing Research, vol 56; 505-520.
