 With the passing of dyslexia laws in the state of New Jersey in 2014, there has been an increased focus on reading disabilities and dyslexia particularly in the area of effective assessment and remediation. More and more parents and health related professionals are looking to understand the components of effective dyslexia testing and who is qualified to perform it. So I decided to write a multi-part series regarding the components of comprehensive dyslexia testing in order to assist parents and professionals to better understand the steps of the testing process.
With the passing of dyslexia laws in the state of New Jersey in 2014, there has been an increased focus on reading disabilities and dyslexia particularly in the area of effective assessment and remediation. More and more parents and health related professionals are looking to understand the components of effective dyslexia testing and who is qualified to perform it. So I decided to write a multi-part series regarding the components of comprehensive dyslexia testing in order to assist parents and professionals to better understand the steps of the testing process.
In this particular post I would like to accomplish two things: dispel several common myths regarding dyslexia testing as well as discuss the first step of SLP based testing which is a language assessment.
Myth 1: Dyslexia can be diagnosed based on a single test!
DYSLEXIA CANNOT BE CONFIRMED BY THE ADMINISTRATION OF ONE SPECIFIC TEST. A comprehensive battery of tests from multiple professionals including neuropsychologists, psychologists, learning specialists, speech-language pathologists and even occupational therapists needs to actually be administered in order to confirm the presence of reading based disabilities.
Myth 2: A doctor can diagnose dyslexia!
A doctor does not have adequate training to diagnose learning disabilities, the same way as a doctor cannot diagnose speech and language problems. Both lie squarely outside of their scope of practice! A doctor can listen to parental concerns and suggest an appropriate plan of action (recommend relevant assessments) but they couldn’t possibly diagnose dyslexia which is made on the basis of team assessments.
Myth 3: Speech Pathologists cannot perform dyslexia testing!
SPEECH-LANGUAGE PATHOLOGISTS TRAINED IN IDENTIFICATION OF READING AND WRITING DISORDERS ARE FULLY QUALIFIED TO PERFORM SIGNIFICANT PORTIONS OF DYSLEXIA BATTERY.
So what are the dyslexia battery components?
Prior to initiating an actual face to face assessment with the child, we need to take down a thorough case history (example HERE) in order to determine any pre-existing risk factors. Dyslexia risk factors may include (but are not limited to):
- History of language and learning difficulties in the family
- History of language delay (impaired memory, attention, grammar, syntax, sentence repetition ability, etc) as well as
- History of impaired phonological awareness skills (difficulty remembering children’s songs, recognizing and making rhymes, confusing words that sound alike, etc).
After that, we need to perform language testing to determine whether the child presents with any deficits in that area. Please note that while children with language impairments are at significant risk for dyslexia not all children with dyslexia present with language impairments. In other words, the child may be cleared by language testing but still present with significant reading disability, which is why comprehensive language testing is only the first step in the dyslexia assessment battery.
 LANGUAGE TESTING
LANGUAGE TESTING
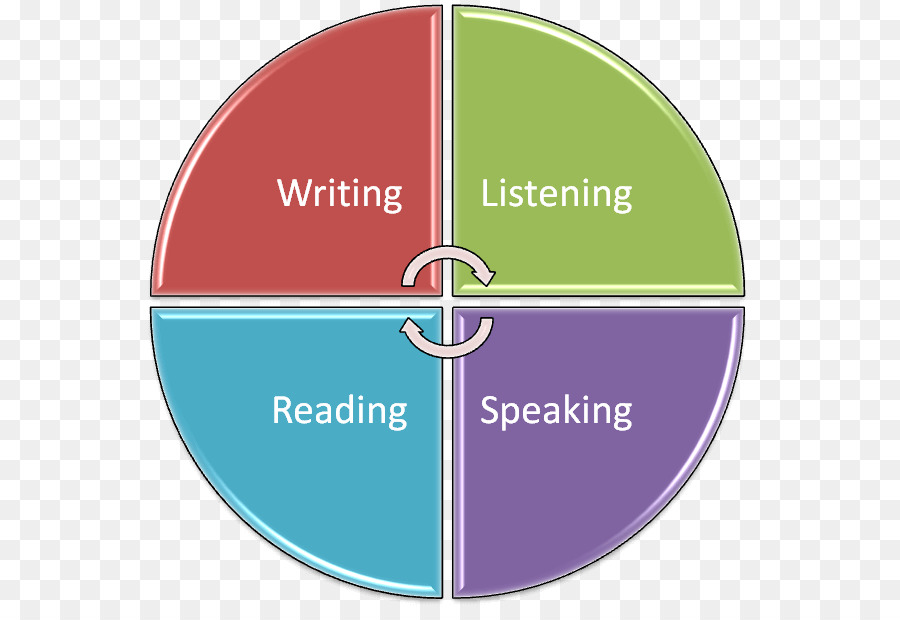
Here we are looking to assess the child’s listening comprehension. processing skills, and verbal expression in the form of conversational and narrative competencies. Oral language is the prerequisite to reading and writing. So a single vocabulary test, a grammar completion task, or even a sentence formulation activity is simply not going to count as a part of a comprehensive assessment.
In children without obvious linguistic deficits such as limited vocabulary, difficulty following directions, or grammatical/syntactic errors (which of course you’ll need to test) I like to use the following tasks, which are sensitive to language impairment:
Listening Comprehension (with a verbal response component)
- Here it is important to assess the student’s ability to listen to short passages and answer a variety of story related questions vs. passively point at 1 of 4 pictures depicting a particular sentence structure (e.g., Point to the picture which shows: “The duck was following the girl”). I personally like to use the Listening Comprehension Tests for this task but any number of subtests from other tests have similar components.
Semantic Flexibility
- Here it is important to assess the student’s vocabulary ability via manipulation of words to create synonyms, antonyms, multiple meaning words, definitions, etc. For this task I like to use the WORD Tests (3-Elementary and 2-Adolescent).
Narrative Production:
- A hugely important part of a language assessment is an informal spontaneously produced narrative sample, which summarizes a book or a movie. Just one few minute narrative sample can yield information on the following:
- Sequencing Ability
- Working Memory
- Grammar
- Vocabulary
- Pragmatics and perspective taking
- Story grammar (Stein & Glenn, 1979)
Usually I don’t like to use any standardized testing for assessment of this skill but use the parameters from the materials I created myself based on existing narrative research (click HERE).
Social Pragmatic Language
- Given my line of work (school in an outpatient psychiatric setting), no testing is complete without some for of social pragmatic language assessment in order to determine whether the student presents with hidden social skill deficits. It is important to note that I’ve seen time and time again students acing the general language testing only to bomb on the social pragmatic tasks which is why this should be a mandatory part of every language test in my eyes. Here, a variety of choices exists. For quick results I typically tends to use the Social Language Development Tests as well as portions of the Social Thinking Dynamic Assessment Protocol®.
Not sure what type of linguistic deficits your student is displaying? Grab a relevant checklist and ask the student’s teacher and parent fill it out (click HERE to see types of available checklists)
So there you have it! The first installment on comprehensive dyslexia testing is complete.
READ part II which discusses components of Phonological Awareness and Word Fluency testing HERE.
Read part III of this series which discusses components of Reading Fluency and Reading Comprehension testing HERE.
 Frequently, I see a variation of the following scenario on many speech and language forums.
Frequently, I see a variation of the following scenario on many speech and language forums. Let’s begin by answering a few simple questions. Was a thorough language evaluation with an emphasis on the child’s social pragmatic language abilities been completed? And by thorough, I am not referring to general language tests but to a variety of formal and informal social pragmatic language testing (read more
Let’s begin by answering a few simple questions. Was a thorough language evaluation with an emphasis on the child’s social pragmatic language abilities been completed? And by thorough, I am not referring to general language tests but to a variety of formal and informal social pragmatic language testing (read more  Please note that none of the general language tests such as the Preschool Language Scale-5 (PLS-5), Comprehensive Assessment of Spoken Language (CASL-2), the Test of Language Development-4 (TOLD-4) or even the Clinical Evaluation of Language Fundamentals Tests (CELF-P2)/ (CELF-5) tap into the child’s social language competence because they do NOT directly test the child’s social language skills (e.g., CELF-5 assesses them via a parental/teachers questionnaire). Thus, many children can attain average scores on these tests yet still present with pervasive social language deficits. That is why it’s very important to thoroughly assess social pragmatic language abilities of all children (no matter what their age is) presenting with behavioral deficits.
Please note that none of the general language tests such as the Preschool Language Scale-5 (PLS-5), Comprehensive Assessment of Spoken Language (CASL-2), the Test of Language Development-4 (TOLD-4) or even the Clinical Evaluation of Language Fundamentals Tests (CELF-P2)/ (CELF-5) tap into the child’s social language competence because they do NOT directly test the child’s social language skills (e.g., CELF-5 assesses them via a parental/teachers questionnaire). Thus, many children can attain average scores on these tests yet still present with pervasive social language deficits. That is why it’s very important to thoroughly assess social pragmatic language abilities of all children (no matter what their age is) presenting with behavioral deficits.







 A few weeks ago I reviewed the
A few weeks ago I reviewed the 









 Today I am very excited to introduce my new product “
Today I am very excited to introduce my new product “ The DSM-5 was released in May 2013 and with it came a revision of criteria for the diagnosis and classification of many psychiatric
The DSM-5 was released in May 2013 and with it came a revision of criteria for the diagnosis and classification of many psychiatric