 I frequently see numerous posts on Facebook that ask group members, “What are your activities/goals for a particular age group (e.g., preschool, middle school, high school, etc.) or a particular disorder (e.g., Down Syndrome)? After seeing these posts appear over and over again in a variety of groups, I decided to write my own post on this topic, explaining why asking such broad questions will not result in optimal therapeutic interventions for the clients in question. Continue reading Dear SLPs, Try Asking This Instead
I frequently see numerous posts on Facebook that ask group members, “What are your activities/goals for a particular age group (e.g., preschool, middle school, high school, etc.) or a particular disorder (e.g., Down Syndrome)? After seeing these posts appear over and over again in a variety of groups, I decided to write my own post on this topic, explaining why asking such broad questions will not result in optimal therapeutic interventions for the clients in question. Continue reading Dear SLPs, Try Asking This Instead
Category: Data
Why “good grades” do not automatically rule out “adverse educational impact”
 As a speech-language pathologist (SLP) working with school-age children, I frequently assess students whose language and literacy abilities adversely impact their academic functioning. For the parents of school-aged children with suspected language and literacy deficits as well as for the SLPs tasked with screening and evaluating them, the concept of ‘academic impact’ comes up on daily basis. In fact, not a day goes by when I do not see a variation of the following question: “Is there evidence of academic impact?”, being discussed in a variety of Facebook groups dedicated to speech pathology issues. Continue reading Why “good grades” do not automatically rule out “adverse educational impact”
As a speech-language pathologist (SLP) working with school-age children, I frequently assess students whose language and literacy abilities adversely impact their academic functioning. For the parents of school-aged children with suspected language and literacy deficits as well as for the SLPs tasked with screening and evaluating them, the concept of ‘academic impact’ comes up on daily basis. In fact, not a day goes by when I do not see a variation of the following question: “Is there evidence of academic impact?”, being discussed in a variety of Facebook groups dedicated to speech pathology issues. Continue reading Why “good grades” do not automatically rule out “adverse educational impact”
Help, My Student has a Huge Score Discrepancy Between Tests and I Don’t Know Why?
 Here’s a familiar scenario to many SLPs. You’ve administered several standardized language tests to your student (e.g., CELF-5 & TILLS). You expected to see roughly similar scores across tests. Much to your surprise, you find that while your student attained somewhat average scores on one assessment, s/he had completely bombed the second assessment, and you have no idea why that happened.
Here’s a familiar scenario to many SLPs. You’ve administered several standardized language tests to your student (e.g., CELF-5 & TILLS). You expected to see roughly similar scores across tests. Much to your surprise, you find that while your student attained somewhat average scores on one assessment, s/he had completely bombed the second assessment, and you have no idea why that happened.
So you go on social media and start crowdsourcing for information from a variety of SLPs located in a variety of states and countries in order to figure out what has happened and what you should do about this. Of course, the problem in such situations is that while some responses will be spot on, many will be utterly inappropriate. Luckily, the answer lies much closer than you think, in the actual technical manual of the administered tests.
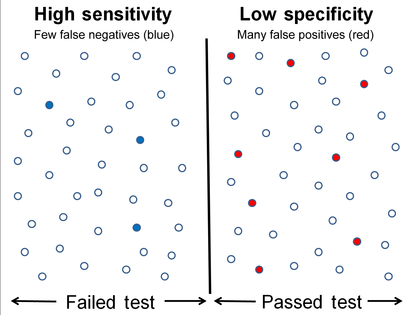
So what is responsible for such as drastic discrepancy? A few things actually. For starters, unless both tests were co-normed (used the same sample of test takers) be prepared to see disparate scores due to the ability levels of children in the normative groups of each test. Another important factor involved in the score discrepancy is how accurately does the test differentiate disordered children from typical functioning ones.
Let’s compare two actual language tests to learn more. For the purpose of this exercise let us select The Clinical Evaluation of Language Fundamentals-5 (CELF-5) and the Test of Integrated Language and Literacy (TILLS). The former is a very familiar entity to numerous SLPs, while the latter is just coming into its own, having been released in the market only several years ago.
Both tests share a number of similarities. Both were created to assess the language abilities of children and adolescents with suspected language disorders. Both assess aspects of language and literacy (albeit not to the same degree nor with the same level of thoroughness). Both can be used for language disorder classification purposes, or can they?
 Actually, my last statement is rather debatable. A careful perusal of the CELF – 5 reveals that its normative sample of 3000 children included a whopping 23% of children with language-related disabilities. In fact, the folks from the Leaders Project did such an excellent and thorough job reviewing its psychometric properties rather than repeating that information, the readers can simply click here to review the limitations of the CELF – 5 straight on the Leaders Project website. Furthermore, even the CELF – 5 developers themselves have stated that: “Based on CELF-5 sensitivity and specificity values, the optimal cut score to achieve the best balance is -1.33 (standard score of 80). Using a standard score of 80 as a cut score yields sensitivity and specificity values of .97. “
Actually, my last statement is rather debatable. A careful perusal of the CELF – 5 reveals that its normative sample of 3000 children included a whopping 23% of children with language-related disabilities. In fact, the folks from the Leaders Project did such an excellent and thorough job reviewing its psychometric properties rather than repeating that information, the readers can simply click here to review the limitations of the CELF – 5 straight on the Leaders Project website. Furthermore, even the CELF – 5 developers themselves have stated that: “Based on CELF-5 sensitivity and specificity values, the optimal cut score to achieve the best balance is -1.33 (standard score of 80). Using a standard score of 80 as a cut score yields sensitivity and specificity values of .97. “
In other words, obtaining a standard score of 80 on the CELF – 5 indicates that a child presents with a language disorder. Of course, as many SLPs already know, the eligibility criteria in the schools requires language scores far below that in order for the student to qualify to receive language therapy services.
In fact, the test’s authors are fully aware of that and acknowledge that in the same document. “Keep in mind that students who have language deficits may not obtain scores that qualify him or her for placement based on the program’s criteria for eligibility. You’ll need to plan how to address the student’s needs within the framework established by your program.”
 But here is another issue – the CELF-5 sensitivity group included only a very small number of: “67 children ranging from 5;0 to 15;11”, whose only requirement was to score 1.5SDs < mean “on any standardized language test”. As the Leaders Project reviewers point out: “This means that the 67 children in the sensitivity group could all have had severe disabilities. They might have multiple disabilities in addition to severe language disorders including severe intellectual disabilities or Autism Spectrum Disorder making it easy for a language disorder test to identify this group as having language disorders with extremely high accuracy. ” (pgs. 7-8)
But here is another issue – the CELF-5 sensitivity group included only a very small number of: “67 children ranging from 5;0 to 15;11”, whose only requirement was to score 1.5SDs < mean “on any standardized language test”. As the Leaders Project reviewers point out: “This means that the 67 children in the sensitivity group could all have had severe disabilities. They might have multiple disabilities in addition to severe language disorders including severe intellectual disabilities or Autism Spectrum Disorder making it easy for a language disorder test to identify this group as having language disorders with extremely high accuracy. ” (pgs. 7-8)
Of course, this begs the question, why would anyone continue to administer any test to students, if its administration A. Does not guarantee disorder identification B. Will not make the student eligible for language therapy despite demonstrated need?
The problem is that even though SLPs are mandated to use a variety of quantitative clinical observations and procedures in order to reliably qualify students for services, standardized tests still carry more value then they should. Consequently, it is important for SLPs to select the right test to make their job easier.
 The TILLS is a far less known assessment than the CELF-5 yet in the few years it has been out on the market it really made its presence felt by being a solid assessment tool due to its valid and reliable psychometric properties. Again, the venerable Dr. Carol Westby had already done such an excellent job reviewing its psychometric properties that I will refer the readers to her review here, rather than repeating this information as it will not add anything new on this topic. The upshot of her review as follows: “The TILLS does not include children and adolescents with language/literacy impairments (LLIs) in the norming sample. Since the 1990s, nearly all language assessments have included children with LLIs in the norming sample. Doing so lowers overall scores, making it more difficult to use the assessment to identify students with LLIs. (pg. 11)”
The TILLS is a far less known assessment than the CELF-5 yet in the few years it has been out on the market it really made its presence felt by being a solid assessment tool due to its valid and reliable psychometric properties. Again, the venerable Dr. Carol Westby had already done such an excellent job reviewing its psychometric properties that I will refer the readers to her review here, rather than repeating this information as it will not add anything new on this topic. The upshot of her review as follows: “The TILLS does not include children and adolescents with language/literacy impairments (LLIs) in the norming sample. Since the 1990s, nearly all language assessments have included children with LLIs in the norming sample. Doing so lowers overall scores, making it more difficult to use the assessment to identify students with LLIs. (pg. 11)”
Now, here many proponents of inclusion of children with language disorders in the normative sample will make a variation of the following claim: “You CANNOT diagnose a language impairment if children with language impairment were not included in the normative sample of that assessment!” Here’s a major problem with such assertion. When a child is referred for a language assessment, we really have no way of knowing if this child has a language impairment until we actually finish testing them. We are in fact attempting to confirm or refute this fact, hopefully via the use of reliable and valid testing. However, if the normative sample includes many children with language and learning difficulties, this significantly affects the accuracy of our identification, since we are interested in comparing this child’s results to typically developing children and not the disordered ones, in order to learn if the child has a disorder in the first place. As per Peña, Spaulding and Plante (2006), “the inclusion of children with disabilities may be at odds with the goal of classification, typically the primary function of the speech pathologist’s assessment. In fact, by including such children in the normative sample, we may be “shooting ourselves in the foot” in terms of testing for the purpose of identifying disorders.”(p. 248)
 Then there’s a variation of this assertion, which I have seen in several Facebook groups: “Children with language disorders score at the low end of normal distribution“. Once again such assertion is incorrect since Spaulding, Plante & Farinella (2006) have actually shown that on average, these kids will score at least 1.28 SDs below the mean, which is not the low average range of normal distribution by any means. As per authors: “Specific data supporting the application of “low score” criteria for the identification of language impairment is not supported by the majority of current commercially available tests. However, alternate sources of data (sensitivity and specificity rates) that support accurate identification are available for a subset of the available tests.” (p. 61)
Then there’s a variation of this assertion, which I have seen in several Facebook groups: “Children with language disorders score at the low end of normal distribution“. Once again such assertion is incorrect since Spaulding, Plante & Farinella (2006) have actually shown that on average, these kids will score at least 1.28 SDs below the mean, which is not the low average range of normal distribution by any means. As per authors: “Specific data supporting the application of “low score” criteria for the identification of language impairment is not supported by the majority of current commercially available tests. However, alternate sources of data (sensitivity and specificity rates) that support accurate identification are available for a subset of the available tests.” (p. 61)
Now, let us get back to your child in question, who performed so differently on both of the administered tests. Given his clinically observed difficulties, you fully expected your testing to confirm it. But you are now more confused than before. Don’t be! Search the technical manual for information on the particular test’s sensitivity and specificity to look up the numbers. Vance and Plante (1994) put forth the following criteria for accurate identification of a disorder (discriminant accuracy): “90% should be considered good discriminant accuracy; 80% to 89% should be considered fair. Below 80%, misidentifications occur at unacceptably high rates” and leading to “serious social consequences” of misidentified children. (p. 21)
Review the sensitivity and specificity of your test/s, take a look at the normative samples, see if anything unusual jumps out at you, which leads you to believe that the administered test may have some issues with assessing what it purports to assess. Then, after supplementing your standardized testing results with good quality clinical data (e.g., narrative samples, dynamic assessment tasks, etc.), consider creating a solidly referenced purchasing pitch to your administration to invest in more valid and reliable standardized tests.
Hope you find this information helpful in your quest to better serve the clients on your caseload. If you are interested in learning more regarding evidence-based assessment practices as well as psychometric properties of various standardized speech-language tests visit the SLPs for Evidence-Based Practice group on Facebook learn more.
References:
- Peña ED, Spaulding TJ, and Plante E. ( 2006) The composition of normative groups and diagnostic decision-making: Shooting ourselves in the foot. American Journal of Speech-Language Pathology 15: 247–54.
- Spaulding, T. J., Plante, E., & Farinella, K. A. (2006). Eligibility criteria for language impairment: Is the low end of normal always appropriate? Language, Speech, and Hearing Services in Schools, 37, 61-72.
- Vance, R., & Plante, E. (1994). Selection of preschool language tests: A data-based approach. Language, Speech, and Hearing Services in Schools, 25, 15-24.
Early Intervention Evaluations PART II: Assessing Suspected Motor Speech Disorders in Children Under 3
In my previous post on this topic, I brought up concerns regarding the paucity of useful information in EI SLP reports for children under 3 years of age and made some constructive suggestions of how that could be rectified. In 2013, I had written about another significant concern, which involved neurodevelopmental pediatricians (rather than SLPs), diagnosing Childhood Apraxia of Speech (CAS), without the adequate level of training and knowledge regarding motor speech disorders. Today, I wanted to combine both topics and delve deeper into another area of EI SLP evaluations, namely, assessments of toddlers with suspected motor speech disorders.
Firstly, it is important to note that CAS is disturbingly overdiagnosed. A cursory review of both parent and professional social media forums quickly reveals that this diagnosis is doled out like candy by both SLPs and medical professionals alike, often without much training and knowledge regarding the disorder in question. The child is under 3, has a limited verbal output coupled with a number of phonological processes, and the next thing you know, s/he is labeled as having Childhood Apraxia of Speech (CAS). But is this diagnosis truly that straightforward?
Let us begin with the fact that all reputable organizations involved in the dissemination of information on the topic of CAS (e.g., ASHA, CASANA, etc.), strongly discourage the diagnosis of CAS in children under three years of age with limited verbal output, and limited time spent in EBP therapy specifically targeting the remediation of motor speech disorders.
 Assessment of motor speech disorders in young children requires solid knowledge and expertise. That is because CAS has a number of overlapping symptoms with other speech sound disorders (e.g., severe phonological disorder, dysarthria, etc). Furthermore, symptoms which may initially appear as CAS may change during the course of intervention by the time the child is older (e.g., 3 years of age) which is why diagnosing toddlers under 3 years of age is very problematic and the use of “suspected” or “working” diagnosis is recommended (Davis & Velleman, 2000) in order to avoid misdiagnosis. Finally, the diagnosis of CAS is also problematic due to the fact that there are still to this day no valid or reliable standardized assessments sensitive to CAS detection (McCauley & Strand, 2008).
Assessment of motor speech disorders in young children requires solid knowledge and expertise. That is because CAS has a number of overlapping symptoms with other speech sound disorders (e.g., severe phonological disorder, dysarthria, etc). Furthermore, symptoms which may initially appear as CAS may change during the course of intervention by the time the child is older (e.g., 3 years of age) which is why diagnosing toddlers under 3 years of age is very problematic and the use of “suspected” or “working” diagnosis is recommended (Davis & Velleman, 2000) in order to avoid misdiagnosis. Finally, the diagnosis of CAS is also problematic due to the fact that there are still to this day no valid or reliable standardized assessments sensitive to CAS detection (McCauley & Strand, 2008).
In March 2017, Dr. Edythe Strand wrote an excellent article for the ASHA Leader entitled: “Appraising Apraxia“, in which she used a case study of a 3-year-old boy to describe how a differential diagnosis for CAS can be performed. She reviewed CAS characteristics, informal assessment protocols, aspects of diagnosis and treatment, and even included ‘Examples of Diagnostic Statements for CAS’ (which illustrate how clinicians can formulate their impressions regarding the child’s strengths and needs without explicitly labeling the child’s diagnosis as CAS).
Today, I’d like to share what information I tend to include in speech-language reports geared towards the assessing motor speech disorders in children under 3 years of age. I have a specific former client in mind for whom a differential diagnosis was particularly needed. Here’s why.
This particular 30-month client, TQ, (I did mention that I get quite a few clients for assessment around that age), was brought in due to parental concerns over her significantly reduced speech and expressive language abilities characterized by unintelligible “babbling-like” utterances and lack of expressive language. All of TQ’s developmental milestones with the exception of speech and language had been achieved grossly at age expectancy. She began limitedly producing word approximations at ~16 months of age but at 30 months of age, her verbal output was still very restricted. She mainly communicated via gestures, pointing, word approximations, and a handful of signs.
Interestingly, as an infant, she had a restricted lingual frenulum. However, since it did not affect her ability to feed, no surgical intervention was needed. Indeed, TQ presented with an adequate lingual movement for both feeding and speech sound production, so her ankyloglossia (or anterior tongue tie) was definitely not the culprit which caused her to have limited speech production.
 Prior to being reevaluated by me, TQ underwent an early intervention assessment at ~26 months of age. She was diagnosed with CAS by an evaluating SLP and was found to be eligible for speech-language services, which she began receiving shortly thereafter. However, Mrs. Q noted that TQ was making very few gains in therapy and her treating SLP was uncertain regarding why her progress in therapy was so limited. Mrs. Q was also rather uncertain that TQ’s diagnosis of CAS was indeed a correct one, which was another reason why she sought a second opinion.
Prior to being reevaluated by me, TQ underwent an early intervention assessment at ~26 months of age. She was diagnosed with CAS by an evaluating SLP and was found to be eligible for speech-language services, which she began receiving shortly thereafter. However, Mrs. Q noted that TQ was making very few gains in therapy and her treating SLP was uncertain regarding why her progress in therapy was so limited. Mrs. Q was also rather uncertain that TQ’s diagnosis of CAS was indeed a correct one, which was another reason why she sought a second opinion.
Assessment of TQ’s social-emotional functioning, play skills, and receptive language (via a combination of Revised Westby Play Scale (Westby, 2000), REEL-3, & PLS-5) quickly revealed that she was a very bright little girl who was developing on target in all of the tested areas. Assessment of TQ’s expressive language (via REEL-3, PLS-5 & LUI*), revealed profoundly impaired, expressive language abilities. But due to which cause?
Despite lacking verbal speech, TQ’s communicative frequency (how often she attempted to spontaneously and appropriately initiate interactions with others), as well as her communicative intent (e.g., gaining attention, making requests, indicating protests, etc), were judged to be appropriate for her age. She was highly receptive to language stimulation given tangible reinforcements and as the assessment progressed she was observed to significantly increase the number and variety of vocalizations and word approximations including delayed imitation of words and sounds containing bilabial and alveolar nasal phonemes.
For the purpose of TQ’s speech assessment, I was interested in gaining knowledge regarding the following:
- Automatic vs. volitional control
- Simple vs. complex speech production
- Consistency of productions on repetitions of the same words/word approximations
- Vowel Productions
- Imitation abilities
- Prosody
- Phonetic inventory
- Phonotactic Constraints
- Stimulability
 TQ’s oral peripheral examination yielded no difficulties with oral movements during non-speaking as well as speaking tasks. She was able to blow bubbles, stick out tongue, smile, etc as well as spontaneously vocalize without any difficulties. Her voice quality, pitch, loudness, and resonance during vocalizations and approximated utterances were judged to be appropriate for age and gender. Her prosody and fluency could not be determined due to lack of spontaneously produced continuous verbal output.
TQ’s oral peripheral examination yielded no difficulties with oral movements during non-speaking as well as speaking tasks. She was able to blow bubbles, stick out tongue, smile, etc as well as spontaneously vocalize without any difficulties. Her voice quality, pitch, loudness, and resonance during vocalizations and approximated utterances were judged to be appropriate for age and gender. Her prosody and fluency could not be determined due to lack of spontaneously produced continuous verbal output.
- Phonetic inventory of all the sounds TQ produced during the assessment is as follows:
- Consonants: plosive nasals (/m/) and alveolars (/t/, /d/, n), as well as a glide (/w/)
- Vowels: (/a/, /e/, /i/, /o/)
- TQ’s phonotactic repertoire was primarily comprised of word approximations restricted to specific sounds and consisted of CV (e.g., ne), VCV (e.g., ada), CVC (e.g., nyam), CVCV (e.g., nada), VCVC (e.g., adat), CVCVCV (nadadi), VCVCV(e.g., adada) syllable shapes
- TQ’s speech intelligibility in known and unknown contexts was profoundly reduced to unfamiliar listeners. However, her word approximations were consistent across all productions.
- Due to the above I could not perform an in-depth phonological processes analysis
However, by this time I had already formulated a working hypothesis regarding TQ’s speech production difficulties. Based on her speech sound assessment TQ presented with severe phonological disorder characterized by restricted sound inventory, simplification of sound sequences, as well as patterns of sound use errors (e.g., predominance of alveolar /d/ and nasal /n/ sounds when attempting to produce most word approximations) in speech (Stoel-Gammon, 1987).
TQ’s difficulties were not consistent with the diagnosis Childhood Apraxia of Speech (CAS) at that time due to the following:
- Adequate and varied production of vowels
- Lack of restricted use of syllables during verbalizations (TQ was observed to make verbalizations up to 3 syllables in length)
- Lack of disruptions in rate, rhythm, and stress of speech
- Frequent and spontaneous use of consistently produced verbalizations
- Lack of verbal groping behaviors when producing word-approximations
- Good control of pitch, loudness and vocal quality during vocalizations
 I felt that the diagnosis of CAS was not applicable because TQ lacked a verbal lexicon and no specific phonological intervention techniques had been trialed with her during the course of her brief therapy (~4 months) to elicit word productions (Davis & Velleman, 2000; Strand, 2003). While her EI speech therapist documented that therapy has primarily focused on ‘oral motor activities to increase TQ’s awareness of her articulators and to increase imitation of oral motor movements’, I knew that until a variety of phonological/motor-speech specific interventions had been trialed over a period of time (at least ~6 months as per Davis & Velleman, 2000) the diagnosis of CAS could not be reliably made.
I felt that the diagnosis of CAS was not applicable because TQ lacked a verbal lexicon and no specific phonological intervention techniques had been trialed with her during the course of her brief therapy (~4 months) to elicit word productions (Davis & Velleman, 2000; Strand, 2003). While her EI speech therapist documented that therapy has primarily focused on ‘oral motor activities to increase TQ’s awareness of her articulators and to increase imitation of oral motor movements’, I knew that until a variety of phonological/motor-speech specific interventions had been trialed over a period of time (at least ~6 months as per Davis & Velleman, 2000) the diagnosis of CAS could not be reliably made.
I still, however, wanted to be cautious as there were a few red flags I had noted which may have potentially indicative of a non-CAS motor speech involvement, due to which I wanted to include some recommendations pertaining to motor speech remediation.
Now it is possible that after 6 months of intensive application of EBP phonological and motor speech approaches TQ would have turned 3 and still presented with highly restricted speech sound inventory and profoundly impaired speech production, making her eligible for the diagnosis of CAS in earnest. However, at the time of my assessment, making such diagnosis in view of all the available evidence would have been both clinically inappropriate and unethical.
So what were my recommendations you may ask? Well, I provisionally diagnosed TQ with a severe phonological disorder and recommended that among a variety of phonologically-based approaches to trial, an EBP approach to the treatment of motor speech disorders be also used with her for a period of 6 months to determine if it would expedite speech gains.
 *For those of you who are interested in the latest EBP treatment for motor speech disorders, current evidence supports the use of the Rapid Syllable Transition Treatment (ReST). ReST is a free EBP treatment developed by the SLPs at the University of Sydney, which uses nonsense words, designed to help children coordinate movements across syllables in long words and phrases as well as helps them learn new speech movements. It is, however, important to note for young children with highly restricted sound inventories, characterized by a lack of syllable production, ReST will not be applicable. For them, the Integral Stimulation/Dynamic Temporal and Tactile Cueing (DTTC) approaches do have some limited empirical support.
*For those of you who are interested in the latest EBP treatment for motor speech disorders, current evidence supports the use of the Rapid Syllable Transition Treatment (ReST). ReST is a free EBP treatment developed by the SLPs at the University of Sydney, which uses nonsense words, designed to help children coordinate movements across syllables in long words and phrases as well as helps them learn new speech movements. It is, however, important to note for young children with highly restricted sound inventories, characterized by a lack of syllable production, ReST will not be applicable. For them, the Integral Stimulation/Dynamic Temporal and Tactile Cueing (DTTC) approaches do have some limited empirical support.
I also made sure to make a note in my report regarding the inappropriate use of non-speech oral motor exercises (NSOMEs) in therapy, indicating that there is NO research to support the use of NSOMEs to stimulate speech production (Lof, 2010).
In addition to the trialing of phonological and motor based approaches I also emphasized the need to establish consistent lexicon via development of functional words needed in daily communication and listed a number of examples across several categories. I made recommendations regarding select approaches and treatment techniques to trial in therapy, as well as suggestions for expansion of sounds and structures. Finally, I made suggestions for long and short term therapy goals for a period of 6 months to trial with TQ in therapy and provided relevant references to support the claims I’ve made in my report.
You may be interested in knowing that nowadays TQ is doing quite well, and at this juncture, she is still, ineligible for the diagnosis CAS (although she needs careful ongoing monitoring with respect to the development of reading difficulties when she is older).
 Now I know that some clinicians will be quick to ask me: “What’s the harm in overdiagnosing CAS if the child’s speech production will still be treated via the application of motor speech production principles?” Well, aside from the fact that it’s obviously unethical and can result in terrifying the parents into obtaining all sorts of questionable and even downright harmful bunk treatments for their children, the treatment may only be limitedly appropriate, and may not result in the best possible outcomes for a particular child. To illustrate, TQ never presented with CAS and as such, while she may have initially limitedly benefited from the application of motor speech principles to address her speech production, shortly thereafter, the application of the principles of the dynamic systems theory is what brought about significant changes in her phonological repertoire.
Now I know that some clinicians will be quick to ask me: “What’s the harm in overdiagnosing CAS if the child’s speech production will still be treated via the application of motor speech production principles?” Well, aside from the fact that it’s obviously unethical and can result in terrifying the parents into obtaining all sorts of questionable and even downright harmful bunk treatments for their children, the treatment may only be limitedly appropriate, and may not result in the best possible outcomes for a particular child. To illustrate, TQ never presented with CAS and as such, while she may have initially limitedly benefited from the application of motor speech principles to address her speech production, shortly thereafter, the application of the principles of the dynamic systems theory is what brought about significant changes in her phonological repertoire.
That is why the correct diagnosis is so important for young children under 3 years of age. But before it can be made, extensive (reputable and evidence supported) training and education are needed by evaluating SLPs on the assessment and treatment of motor speech disorders in young children.
References:
- Davis, B & Velleman, S (2000). Differential diagnosis and treatment of developmental apraxia of speech in infants and toddlers”. The Transdisciplinary Journal. 10 (3): 177 – 192.
- Lof, G., & Watson, M. (2010). Five reasons why nonspeech oral-motor exercises do not work. Perspectives on School-Based Issues, 11.109-117.
- McCauley RJ, Strand EA. (2008). A Review of Standardized Tests of Nonverbal Oral and Speech Motor Performance in Children. American Journal of Speech-Language Pathology, 17,81-91.
- McCauley R.J., Strand E., Lof, G.L., Schooling T. & Frymark, T. (2009). Evidence-Based Systematic Review: Effects of Nonspeech Oral Motor Exercises on Speech, American Journal of Speech-Language Pathology, 18, 343-360.
- Murray, E., McCabe, P. & Ballard, K.J. (2015). A Randomized Control Trial of Treatments for Childhood Apraxia of Speech. Journal of Speech, Language and Hearing Research 58 (3) 669-686.
- Stoel-Gammon, C. (1987). Phonological skills of 2-year-olds. Language, Speech, and Hearing Services in Schools, 18, 323-329.
- Strand, E (2003). Childhood apraxia of speech: suggested diagnostic markers for the young child. In Shriberg, L & Campbell, T (Eds) Proceedings of the 2002 childhood apraxia of speech research symposium. Carlsbad, CA: Hendrix Foundation.
- Strand, E, McCauley, R, Weigand, S, Stoeckel, R & Baas, B (2013) A Motor Speech Assessment for Children with Severe Speech Disorders: Reliability and Validity Evidence. Journal of Speech Language and Hearing Research, vol 56; 505-520.
Early Intervention Evaluations PART I: Assessing 2.5 year olds
 Today, I’d like to talk about speech and language assessments of children under three years of age. Namely, the quality of these assessments. Let me be frank, I am not happy with what I am seeing. Often times, when I receive a speech-language report on a child under three years of age, I am struck by how little functional information it contains about the child’s linguistic strengths and weaknesses. Indeed, conversations with parents often reveal that at best the examiner spent no more than half an hour or so playing with the child and performed very limited functional testing of their actual abilities. Instead, they interviewed the parent and based their report on parental feedback alone. Consequently, parents often end up with a report of very limited value, which does not contain any helpful information on how delayed is the child as compared to peers their age.
Today, I’d like to talk about speech and language assessments of children under three years of age. Namely, the quality of these assessments. Let me be frank, I am not happy with what I am seeing. Often times, when I receive a speech-language report on a child under three years of age, I am struck by how little functional information it contains about the child’s linguistic strengths and weaknesses. Indeed, conversations with parents often reveal that at best the examiner spent no more than half an hour or so playing with the child and performed very limited functional testing of their actual abilities. Instead, they interviewed the parent and based their report on parental feedback alone. Consequently, parents often end up with a report of very limited value, which does not contain any helpful information on how delayed is the child as compared to peers their age.
So today I like to talk about what information should such speech-language reports should contain. For the purpose of this particular post, I will choose a particular developmental age at which children at risk of language delay are often assessed by speech-language pathologists. Below you will find what information I typically like to include in these reports as well as developmental milestones for children 30 months or 2.5 years of age.
 Why 30 months, you may ask? Well, there isn’t really any hard science to it. It’s just that I noticed that a significant percentage of parents who were already worried about their children’s speech-language abilities when they were younger, begin to act upon those worries as the child is nearing 3 years of age and their abilities are not improving or are not commensurate with other peers their age.
Why 30 months, you may ask? Well, there isn’t really any hard science to it. It’s just that I noticed that a significant percentage of parents who were already worried about their children’s speech-language abilities when they were younger, begin to act upon those worries as the child is nearing 3 years of age and their abilities are not improving or are not commensurate with other peers their age.
So here is the information I include in such reports (after I’ve gathered pertinent background information in the form of relevant intakes and questionnaires, of course). Naturally, detailed BACKGROUND HISTORY section is a must! Prenatal, perinatal, and postnatal development should be prominently featured there. All pertinent medical history needs to get documented as well as all of the child’s developmental milestones in the areas of cognition, emotional development, fine and gross motor function, and of course speech and language. Here, I also include a family history of red flags: international or domestic adoption of the child (if relevant) as well as familial speech and language difficulties, intellectual impairment, psychiatric disorders, special education placements, or documented deficits in the areas of literacy (e.g., reading, writing, and spelling). After all, if any of the above issues are present in isolation or in combination, the risk for language and literacy deficits increases exponentially, and services are strongly merited for the child in question.
For bilingual children, the next section will cover LANGUAGE BACKGROUND AND USE. Here, I describe how many and which languages are spoken in the home and how well does the child understand and speak any or all of these languages (as per parental report based on questionnaires).
After that, I move on to describe the child’s ADAPTIVE BEHAVIOR during the assessment. In this section, I cover emotional relatedness, joint attention, social referencing, attention skills, communicative frequency, communicative intent, communicative functions, as well as any and all unusual behaviors noted during the therapy session (e.g., refusal, tantrums, perseverations, echolalia, etc.) Then I move on to PLAY SKILLS. For the purpose of play assessment, I use the Revised Westby Play Scale (Westby, 2000). In this section, I describe where the child is presently with respect to play skills, and where they actually need to be developmentally (excerpt below).
“During today’s assessment, LS’s play skills were judged to be significantly reduced for his age. A child of LS’s age (30 months) is expected to engage in a number of isolated pretend play activities with realistic props to represent daily experiences (playing house) as well as less frequently experienced events (e.g., reenacting a doctor’s visit, etc.) (corresponds to Stage VI on the Westby Play Scale, Revised Westby Play Scale (Westby, 2000)). Contrastingly, LS presented with limited repertoire routines, which were characterized primarily by exploration of toys, such as operating simple cause and effect toys (given modeling) or taking out and then putting back in playhouse toys. LS’s parents confirmed that the above play schemas were representative of play interactions at home as well. Today’s LS’s play skills were judged to be approximately at Stage II (13 – 17 months) on the Westby Play Scale, (Revised Westby Play Scale (Westby, 2000)) which is significantly reduced for a child of LS’s age, since it is almost approximately ±15 months behind his peers. Thus, based on today’s play assessment, LS’s play skills require therapeutic intervention. “
Sections on AUDITORY FUNCTION, PERIPHERAL ORAL MOTOR EXAM, VOCAL PARAMETERS, FLUENCY AND RESONANCE (and if pertinent FEEDING and SWALLOWING follow) (more on that in another post).
Now, it’s finally time to get to the ‘meat and potatoes’ of the report ARTICULATION AND PHONOLOGY as well as RECEPTIVE and EXPRESSIVE LANGUAGE (more on PRAGMATIC ASSESSMENT in another post).
First, here’s what I include in the ARTICULATION AND PHONOLOGY section of the report.
- Phonetic inventory: all the sounds the child is currently producing including (short excerpt below):
- Consonants: plosive (/p/, /b/, /m/), alveolar (/t/, /d/), velar (/k/, /g/), glide (/w/), nasal (/n/, /m/) glottal (/h/)
- Vowels and diphthongs: ( /a/, /e/, /i/, /o/, /u/, /ou/, /ai/)
- Phonotactic repertoire: What type of words comprised of how many syllables and which consonant-vowel variations the child is producing (excerpt below)
- LS primarily produced one syllable words consisting of CV (e.g., ke, di), CVC (e.g., boom), VCV (e.g., apo) syllable shapes, which is reduced for a child his age.
- Speech intelligibility in known and unknown contexts
- Phonological processes analysis
Now that I have described what the child is capable of speech-wise, I discuss where the child needs to be developmentally:
“A child of LS’s age (30 months) is expected to produce additional consonants in initial word position (k, l, s, h), some consonants (t, d, m, n, s, z) in final word position (Watson & Scukanec, 1997b), several consonant clusters (pw, bw, -nd, -ts) (Stoel-Gammon, 1987) as well as evidence a more sophisticated syllable shape structure (e.g., CVCVC) Furthermore, a 30 month old child is expected to begin monitoring and repairing own utterances, adjusting speech to different listeners, as well as practicing sounds, words, and early sentences (Clark, adapted by Owens, 1996, p. 386) all of which LS is not performing at this time. Based on above developmental norms, LS’s phonological abilities are judged to be significantly below age-expectancy at this time. Therapy is recommended in order to improve LS’s phonological skills.”
 At this point, I am ready to move on to the language portion of the assessment. Here it is important to note that a number of assessments for toddlers under 3 years of age contain numerous limitations. Some such as REEL-3 or Rosetti (a criterion-referenced vs. normed-referenced instrument) are observational or limitedly interactive in nature, while others such as PLS-5, have a tendency to over inflate scores, resulting in a significant number of children not qualifying for rightfully deserved speech-language therapy services. This is exactly why it’s so important that SLPs have a firm knowledge of developmental milestones! After all, after they finish describing what the child is capable of, they then need to describe what the developmental expectations are for a child this age (excerpts below).
At this point, I am ready to move on to the language portion of the assessment. Here it is important to note that a number of assessments for toddlers under 3 years of age contain numerous limitations. Some such as REEL-3 or Rosetti (a criterion-referenced vs. normed-referenced instrument) are observational or limitedly interactive in nature, while others such as PLS-5, have a tendency to over inflate scores, resulting in a significant number of children not qualifying for rightfully deserved speech-language therapy services. This is exactly why it’s so important that SLPs have a firm knowledge of developmental milestones! After all, after they finish describing what the child is capable of, they then need to describe what the developmental expectations are for a child this age (excerpts below).
RECEPTIVE LANGUAGE
“LS’s receptive language abilities were judged to be scattered between 11-17 months of age (as per clinical observations as well as informal PLS-5 and REEL-3 findings), which is also consistent with his play skills abilities (see above). During the assessment LS was able to appropriately understand prohibitive verbalizations (e.g., “No”, “Stop”), follow simple 1 part directions (when repeated and combined with gestures), selectively attend to speaker when his name was spoken (behavioral), perform a routine activity upon request (when combined with gestures), retrieve familiar objects from nearby (when provided with gestures), identify several major body parts (with prompting) on a doll only, select a familiar object when named given repeated prompting, point to pictures of familiar objects in books when named by adult, as well as respond to yes/no questions by using head shakes and head nods. This is significantly below age-expectancy.
A typically developing child 30 months of age is expected to spontaneously follow (without gestures, cues or prompts) 2+ step directives, follow select commands that require getting objects out of sight, answer simple “wh” questions (what, where, who), understand select spatial concepts, (in, off, out of, etc), understand select pronouns (e.g., me, my, your), identify action words in pictures, understand concept sizes (‘big’, ‘little’), identify simple objects according to their function, identify select clothing items such as shoes, shirt, pants, hat (on self or caregiver) as well as understand names of farm animals, everyday foods, and toys. Therapeutic intervention is recommended in order to increase LS’s receptive language abilities.
EXPRESSIVE LANGUAGE:
“During today’s assessment, LS’s expressive language skills were judged to be scattered between 10-15 months of age (as per clinical observations as well as informal PLS-5 and REEL-3 findings). LS was observed to communicate primarily via proto-imperative gestures (requesting and object via eye gaze, reaching) as well as proto-declarative gestures (showing an object via eye gaze, reaching, and pointing). Additionally, LS communicated via vocalizations, head nods, and head shakes. According to parental report, at this time LS’s speaking vocabulary consists of approximately 15-20 words (see word lists below). During the assessment LS was observed to spontaneously produce a number of these words when looking at a picture book, playing with toys, and participating in action based play activities with Mrs. S and clinician. LS was also observed to produce a number of animal sounds when looking at select picture books and puzzles. For therapy planning purposes, it is important to note that LS was observed to imitate more sounds and words, when they were supported by action based play activities (when words and sounds were accompanied by a movement initiated by clinician and then imitated by LS). Today LS was observed to primarily communicate via a very limited number of imitated and spontaneous one word utterances that labeled basic objects and pictures in his environment, which is significantly reduced for his age.
A typically developing child of LS’s chronological age (30 months) is expected to possess a minimum vocabulary of 200+ words (Rescorla, 1989), produce 2-4 word utterance combinations (e.g., noun + verb, verb + noun + location, verb + noun + adjective, etc), in addition to asking 2-3 word questions as well as maintaining a topic for 2+ conversational turns. Therapeutic intervention is recommended in order to increase LS’s expressive language abilities.”
Here you have a few speech-language evaluation excerpts which describe not just what the child is capable of but where the child needs to be developmentally. Now it’s just a matter of summarizing my IMPRESSIONS (child’s strengths and needs), RECOMMENDATIONS as well as SUGGESTED (long and short term) THERAPY GOALS. Now the parents have some understanding regarding their child’s strengths and needs. From here, they can also track their child’s progress in therapy as they now have some idea to what it can be compared to.
 Now I know that many of you will tell me, that this is a ‘perfect world’ evaluation conducted by a private therapist with an unlimited amount of time on her hands. And to some extent, many of you will be right! Yes, such an evaluation was a result of more than 30 minutes spent face-to-face with the child. All in all, it took probably closer to 90 minutes of face to face time to complete it and a few hours to write. And yes, this is a luxury only a few possess and many therapists in the early intervention system lack. But in the long run, such evaluations pay dividends not only, obviously, to your clients but to SLPs who perform them. They enhance and grow your reputation as an evaluating therapist. They even make sense from a business perspective. If you are well-known and highly sought after due to your evaluating expertise, you can expect to be compensated for your time, accordingly. This means that if you decide that your time and expertise are worth private pay only (due to poor insurance reimbursement or low EI rates), you can be sure that parents will learn to appreciate your thoroughness and will choose you over other providers.
Now I know that many of you will tell me, that this is a ‘perfect world’ evaluation conducted by a private therapist with an unlimited amount of time on her hands. And to some extent, many of you will be right! Yes, such an evaluation was a result of more than 30 minutes spent face-to-face with the child. All in all, it took probably closer to 90 minutes of face to face time to complete it and a few hours to write. And yes, this is a luxury only a few possess and many therapists in the early intervention system lack. But in the long run, such evaluations pay dividends not only, obviously, to your clients but to SLPs who perform them. They enhance and grow your reputation as an evaluating therapist. They even make sense from a business perspective. If you are well-known and highly sought after due to your evaluating expertise, you can expect to be compensated for your time, accordingly. This means that if you decide that your time and expertise are worth private pay only (due to poor insurance reimbursement or low EI rates), you can be sure that parents will learn to appreciate your thoroughness and will choose you over other providers.
So, how about it? Can you give it a try? Trust me, it’s worth it!
Selected References:
- Owens, R. E. (1996). Language development: An introduction (4th ed.). Boston, MA: Allyn & Bacon.
- Rescorla, L. (1989). The Language Development Survey: A screening tool for delayed language in toddlers. Journal of Speech and Hearing Disorders, 54, 587–599.
- Selby, J. C., Robb, M. P., & Gilbert, H. R. (2000). Normal vowel articulations between 15 and 36 months of age. Clinical Linguistics and Phonetics, 14, 255-266.
- Stoel-Gammon, C. (1987). Phonological skills of 2-year-olds. Language, Speech, and Hearing Services in Schools, 18, 323-329.
- Watson, M. M., & Scukanec, G. P. (1997b). Profiling the phonological abilities of 2-year-olds: A longitudinal investigation. Child Language Teaching and Therapy, 13, 3-14.
For more information on EI Assessments click on any of the below posts:
- Part II: Early Intervention Evaluations PART II: Assessing Suspected Motor Speech Disorders in Children Under 3
- Part III: Early Intervention Evaluations PART III: Assessing Children Under 2 Years of Age
- Part IV: Early Intervention Evaluations PART IV:Assessing Social Pragmatic Abilities of Children Under 3
The Limitations of Using Total/Core Scores When Determining Speech-Language Eligibility
 In both of the settings where I work, psychiatric outpatient school as well as private practice, I spend a fair amount of time reviewing speech language evaluation reports. As I’m looking at these reports I am seeing that many examiners choose to base their decision making with respect to speech language services eligibility on the students’ core, index, or total scores, which are composite scores. For those who are not familiar with this term, composite scores are standard scores based on the sum of various test scaled scores.
In both of the settings where I work, psychiatric outpatient school as well as private practice, I spend a fair amount of time reviewing speech language evaluation reports. As I’m looking at these reports I am seeing that many examiners choose to base their decision making with respect to speech language services eligibility on the students’ core, index, or total scores, which are composite scores. For those who are not familiar with this term, composite scores are standard scores based on the sum of various test scaled scores.
When the student displays average abilities on all of the presented subtests, use of composite scores clearly indicates that the child does not present with deficits and thereby is not eligible for therapy services.
The same goes for the reverse, when the child is displaying a pattern of deficits which places their total score well below the average range of functioning. Again, it indicates that the child is performing poorly and requires therapy services.
However, there’s also a the third scenario, which presents a cause for concern namely, when the students display a pattern of strengths and weaknesses on a variety of subtests, but end up with an average/low average total scores, making them ineligible for services.
Results of the Test of Problem Solving -2 Elementary (TOPS-3)
| Subtests | Raw Score | Standard Score | Percentile Rank | Description |
| Making Inferences | 19 | 83 | 12 | Below Average |
| Sequencing | 22 | 86 | 17 | Low Average |
| Negative Questions | 21 | 95 | 38 | Average |
| Problem Solving | 21 | 90 | 26 | Average |
| Predicting | 18 | 92 | 29 | Average |
| Determining Causes | 13 | 82 | 11 | Below Average |
| Total Test | 114 | 86 | 18 | Low Average |
Results of the Test of Reading Comprehension-Fourth Edition (TORC-4)
| Subtests | Raw Score | Standard Score | Percentile Rank | Description |
| Relational Vocabulary | 24 | 9 | 37 | Average |
| Sentence Completion | 25 | 9 | 37 | Average |
| Paragraph Construction | 41 | 12 | 75 | Average |
| Text Comprehension | 21 | 7 | 16 | Below Average |
| Contextual Fluency | 86 | 6 | 9 | Below Average |
| Reading Comprehension Index | 90 | Average | ||
The above tables, taken from different evaluations, perfectly illustrate such a scenario. While we see that their total/index scores are within average range, the first student has displayed a pattern of strengths and weaknesses across various subtests of the TOPS-3, while the second one displayed a similar performance pattern on the TORC-4.
Typically in such cases, clinical judgment dictates a number of options:
- Administration of another standardized test further probing into related areas of difficulty (e.g., in such situations the administration of a social pragmatic standardized test may reveal a significant pattern of weaknesses which would confirm student’s eligibility for language therapy services).
- Administration of informal/dynamic assessments/procedures further probing into the student’s critical thinking/verbal reasoning skills.
 Here is the problem though: I only see the above follow-up steps in a small percentage of cases. In the vast majority of cases in which score discrepancies occur, I see the examiners ignoring the weaknesses without follow up. This of course results in the child not qualifying for services.
Here is the problem though: I only see the above follow-up steps in a small percentage of cases. In the vast majority of cases in which score discrepancies occur, I see the examiners ignoring the weaknesses without follow up. This of course results in the child not qualifying for services.
So why do such practices frequently take place? Is it because SLPs want to deny children services? And the answer is NOT at all! The vast majority of SLPs, I have had the pleasure interacting with, are deeply caring and concerned individuals, who only want what’s best for the student in question. Oftentimes, I believe the problem lies with the misinterpretation of/rigid adherence to the state educational code.
For example, most NJ SLPs know that the New Jersey State Education Code dictates that initial eligibility must be determined via use of two standardized tests on which the student must perform 1.5 standard deviations below the mean (or below the 10th percentile). Based on such phrasing it is reasonable to assume that any child who receives the total scores on two standardized tests above the 10th percentile will not qualify for services. Yet this is completely incorrect!
Let’s take a closer look at the clarification memo issued on October 6, 2015, by the New Jersey Department of Education, in response to NJ Edu Code misinterpretation. Here is what it actually states.
“In accordance with this regulation, when assessing for a language disorder for purposes of determining whether a student meets the criteria for communication impaired, the problem must be demonstrated through functional assessment of language in other than a testing situation and performance below 1.5 standard deviations, or the 10th percentile on at least two standardized language tests, where such tests are appropriate, one of which shall be a comprehensive test of both receptive and expressive language.”
“When implementing the requirement with respect to “standardized language tests,” test selection for evaluation or reevaluation of an individual student is based on various factors, including the student’s ability to participate in the tests, the areas of suspected language difficulties/deficits (e.g., morphology, syntax, semantics, pragmatics/social language) and weaknesses identified during the assessment process which require further testing, etc. With respect to test interpretation and decision-making regarding eligibility for special education and related services and eligibility for speech-language services, the criteria in the above provision do not limit the types of scores that can be considered (e.g., index, subtest, standard score, etc.).”
Firstly, it emphasizes functional assessments. It doesn’t mean that assessments should be exclusively standardized rather it emphasizes the best appropriate procedures for the student in question be they standardized and nonstandardized.
Secondly, it does not limit standardized assessment to 2 tests only. Rather it uses though phrase “at least” to emphasize the minimum of tests needed.
It explicitly makes a reference to following up on any weaknesses displayed by the students during standardized testing in order to get to the root of a problem.
It specifies that SLPs must assess all displayed areas of difficulty (e.g., social communication) rather than assessing general language abilities only.
Finally, it explicitly points out that SLPs cannot limit their testing interpretation to the total scores but must to look at the testing results holistically, taking into consideration the student’s entire assessment performance.
The problem is that if SLPs only look at total/core scores then numerous children with linguistically-based deficits will fall through the cracks. We are talking about children with social communication deficits, children with reading disabilities, children with general language weaknesses, etc. These students may be displaying average total scores but they may also be displaying significant subtest weaknesses. The problem is that unless these weaknesses are accounted for and remediated as they are not going to magically disappear or resolve on their own. In fact both research and clinical judgment dictates that these weaknesses will exacerbate over time and will continue to adversely impact both social communication and academics.
 So the next time you see a pattern of strengths and weaknesses and testing, even if it amounts to a total average score, I urge you to dig deeper. I urge you to investigate why this pattern is displayed in the first place. The same goes for you – parents! If you are looking at average total scores but seeing unexplained weaknesses in select testing areas, start asking questions! Ask the professional to explain why those deficits are occuring and tell them to dig deeper if you are not satisfied with what you are hearing. All students deserve access to FAPE (Free and Appropriate Public Education). This includes access to appropriate therapies, they may need in order to optimally function in the classroom.
So the next time you see a pattern of strengths and weaknesses and testing, even if it amounts to a total average score, I urge you to dig deeper. I urge you to investigate why this pattern is displayed in the first place. The same goes for you – parents! If you are looking at average total scores but seeing unexplained weaknesses in select testing areas, start asking questions! Ask the professional to explain why those deficits are occuring and tell them to dig deeper if you are not satisfied with what you are hearing. All students deserve access to FAPE (Free and Appropriate Public Education). This includes access to appropriate therapies, they may need in order to optimally function in the classroom.
I urge my fellow SLP’s to carefully study their respective state codes as well as know who they are state educational representatives are. These are the professionals SLPs can contact with questions regarding educational code clarification. For example, the SEACDC Consultant for the state of New Jersey is currently Fran Liebner (phone: 609-984-4955; Fax: 609-292-5558; e-mail: fran.leibner@doe.state.nj.us).
However, the Department of Education is not the only place SLPs can contact in their state. Numerous state associations worked diligently on behalf of SLPs by liaising with the departments of education in order to have access to up to date information pertaining to school services. ASHA also helpfully provides contact information by state HERE.
When it comes to score interpretation, there are a variety of options available to SLPs in addition to the detailed reading of the test manual. We can use them to ensure that the students we serve experience optimal success in both social and academic settings.
Helpful Smart Speech Therapy Resources:
Show me the Data or Why I Hate the Phrase: “It’s Not So Bad”
 A few days ago I was asked by my higher-ups for a second opinion on a consult regarding a psychological evaluation on an 11-year-old boy, which was depicting a certain pattern of deficits without a reasonable justification as to why they were occurring. I had a working hypothesis but needed more evidence to turn it into a viable theory. So I set out to collect more evidence by interviewing a few ancillary professionals who were providing therapy services to the student.
A few days ago I was asked by my higher-ups for a second opinion on a consult regarding a psychological evaluation on an 11-year-old boy, which was depicting a certain pattern of deficits without a reasonable justification as to why they were occurring. I had a working hypothesis but needed more evidence to turn it into a viable theory. So I set out to collect more evidence by interviewing a few ancillary professionals who were providing therapy services to the student.
The first person I interviewed was his OT, whom I asked regarding the quality of his graphomotor skills. She responded: “Oh, they are not so bad”.
I was perplexed to say the least. What does that mean I asked her. She responded back with: “He can write.”
“But I am not asking you whether he can write”, I responded back. “I am asking you to provide data that will indicate whether his visual perceptual skills, orthographic coding, motor planning and execution, kinesthetic feedback, as well as visual motor coordination, are on par or below those of his grade level peers.”
Needless to say this student graphomotor abilities were nowhere near those of his peers. The below “sample” took me approximately 12 minutes to elicit and required numerous prompts from myself as well as self-corrections from the student to produce.
 This got me thinking of all the parents and professionals who hear litotes such as “It’s not so bad”, or overgeneralized phrases such as: “Her social skills are fine“, “He is functioning higher than what the testing showed“,”He can read“, etc., on daily basis, instead of being provided with detailed data regarding the student’s present level of functioning in a particular academic area.
This got me thinking of all the parents and professionals who hear litotes such as “It’s not so bad”, or overgeneralized phrases such as: “Her social skills are fine“, “He is functioning higher than what the testing showed“,”He can read“, etc., on daily basis, instead of being provided with detailed data regarding the student’s present level of functioning in a particular academic area.
This has to stop, right now!
If you are an educational or health professional who has a habit of making such statements – beware! You are not doing yourself any favors by saying it and you can actually get into some pretty hot water if you are ever involved in a legal dispute.
Here’s why:
These statements are meaningless!
They signify nothing! Let’s use a commonly heard phrase: “He can read.” Sounds fairly simple, right?
Wrong!
In order to make this “loaded” statement, a professional actually needs to understand what the act of reading entails. The act of reading contains a number of active components:
- Phonemic Awareness
- Phonotactic Knowledge
- Rate
- Accuracy
- Fluency
- Vocabulary
- Comprehension
In other words if the child can decode all the words on the page, but their reading rate is slow and labored, then they cannot read!
If the child is a fast but inaccurate reader and has trouble decoding new words then they’re not a reader either!
If the child reads everything quickly and accurately but comprehends very little then they are also not a reader!
Let us now examine another loaded statement, I’ve heard recently for a fellow SLP: “His skills are higher than your evaluation depicted.” Again, what does that mean? Do you have audio, video, or written documentation to support your assertion? No professional should ever make that statement without having detailed data to support it. Otherwise, you will be hearing: “SHOW ME THE DATA!“

These statements are harmful!
They imply to parents that the child is doing relatively well as compared to peers when nothing could be further from the truth! As a good friend and colleague, Maria Del Duca of Communication Station Blog has stated: [By making these comments] “We begin to accept a range of behavior we believe is acceptable for no other reason than we have made that decision. With this idea of mediocrity we limit our client’s potential by unconsciously lowering the bar.”
You might as well be making comments such as: “Well, it’s as good as it going to get”, indicating that the child’s genetic predestination “imposes limits on what a child might achieve” (Walz Garrett, 2012 pg. 30)
These statements are subjective!
They fail to provide any objective evidence such as type of skills addressed within a subset of abilities, percentage of accuracy achieved, number of trials needed, or number of cues and prompts given to the child in order to achieve the aforementioned accuracy.
These statements make you look unprofessional!
I can’t help but laugh when I review progress reports with the following comments:
Social Communication: Johnny is a pleasant child who much more readily interacted with his peers during the present progress reporting period.
What on earth does that mean? What were Johnny’s specific social communication goals? Was he supposed to initiate conversations more frequently with peers? Was he supposed to acknowledge in some way that his peers actually exist on the same physical plane? Your guess is as good as mine!
Reading: Johnny is more willing to read short stories at this time.
Again, what on earth does that mean? What type of text can Johnny now decode? Which consonant digraphs can he consistently recognize in text? Can he differentiate between long and short vowels in CVC and CVCV words such as /bit/ and /bite/? I have no clue because none of that was included in his report.
These statements can cause legal difficulties!
I don’t know about your graduate preparation but I’m pretty sure that most diagnostics professors, repeatedly emphasized to the graduate SLP students the importance of professional record-keeping. Every professor in my acquaintance has that story – the one where they had to go to court and only their detailed scrupulous record-keeping has kept them from crying and cowering from the unrelenting verbal onslaught of the plaintiff’s educational attorney.
Ironically this is exactly what’s going to happen if you keep making these statements and have no data to support your client’s present level of functioning! Legal disputes between parents of developmentally/language impaired children and districts occur at an alarming rate throughout United States; most often over perceived educational deprivation and lack of access to FAPE (Free and Appropriate Education). I would not envy any educational/health related professional who is caught in the middle of these cases lacking data to support appropriate service provision to the student in question.
Conclusion:
So there you have it! These are just a few (of many) reasons why I loathe the phrase: “It’s Not So Bad”. The bottom line is that this vague and subjective statement does a huge disservice to our students as individuals and to us as qualified and competent professionals. So the next time it’s on the tip of your tongue: “Just don’t say it!” And if you are on the receiving end of it, just calmly ask the professional making that statement: “Show me the data!”
