 Lately, I’ve been seeing more and more posts on social media asking for testing suggestions for students who exhibit subtle language-based difficulties. Many of these children are typically referred for initial assessments or reassessments as part of advocate/attorney involved cases, while others are being assessed due to the parental insistence that something “is not quite right” with their language and literacy abilities, even in the presence of “good grades.” Continue reading Comprehensive Assessment of Elementary Aged Children with Subtle Language and Literacy Deficits
Lately, I’ve been seeing more and more posts on social media asking for testing suggestions for students who exhibit subtle language-based difficulties. Many of these children are typically referred for initial assessments or reassessments as part of advocate/attorney involved cases, while others are being assessed due to the parental insistence that something “is not quite right” with their language and literacy abilities, even in the presence of “good grades.” Continue reading Comprehensive Assessment of Elementary Aged Children with Subtle Language and Literacy Deficits
Category: Differential Diagnosis
Neuropsychological or Language/Literacy: Which Assessment is Right for My Child?
![]() Several years ago I began blogging on the subject of independent assessments in speech pathology. First, I wrote a post entitled “Special Education Disputes and Comprehensive Language Testing: What Parents, Attorneys, and Advocates Need to Know“, in which I used 4 different scenarios to illustrate the importance of comprehensive language evaluations for children with subtle language and learning needs. Then I wrote about: “What Makes an Independent Speech-Language-Literacy Evaluation a GOOD Evaluation?” in order to elucidate on what actually constitutes a good independent comprehensive assessment. Continue reading Neuropsychological or Language/Literacy: Which Assessment is Right for My Child?
Several years ago I began blogging on the subject of independent assessments in speech pathology. First, I wrote a post entitled “Special Education Disputes and Comprehensive Language Testing: What Parents, Attorneys, and Advocates Need to Know“, in which I used 4 different scenarios to illustrate the importance of comprehensive language evaluations for children with subtle language and learning needs. Then I wrote about: “What Makes an Independent Speech-Language-Literacy Evaluation a GOOD Evaluation?” in order to elucidate on what actually constitutes a good independent comprehensive assessment. Continue reading Neuropsychological or Language/Literacy: Which Assessment is Right for My Child?
Help, My Child is Receiving All These Therapies But It’s NOT Helping
 On a daily basis I receive emails and messages from concerned parents and professionals, which read along these lines: “My child/student has been diagnosed with: dyslexia, ADHD, APD etc., s/he has been receiving speech, OT, vision, biofeedback, music therapies, etc. but nothing seems to be working.”
On a daily basis I receive emails and messages from concerned parents and professionals, which read along these lines: “My child/student has been diagnosed with: dyslexia, ADHD, APD etc., s/he has been receiving speech, OT, vision, biofeedback, music therapies, etc. but nothing seems to be working.”
Up until now, I have been providing individualized responses to such queries, however, given the unnerving similarity of all the received messages, today I decided to write this post, so other individuals with similar concerns can see my response. Continue reading Help, My Child is Receiving All These Therapies But It’s NOT Helping
What Makes an Independent Speech-Language-Literacy Evaluation a GOOD Evaluation?
 Three years ago I wrote a blog post entitled: “Special Education Disputes and Comprehensive Language Testing: What Parents, Attorneys, and Advocates Need to Know“. In it, I used 4 very different scenarios to illustrate the importance of comprehensive language evaluations for children with subtle language and learning needs. Today I would like to expound more on that post in order to explain, what actually constitutes a good independent comprehensive assessment. Continue reading What Makes an Independent Speech-Language-Literacy Evaluation a GOOD Evaluation?
Three years ago I wrote a blog post entitled: “Special Education Disputes and Comprehensive Language Testing: What Parents, Attorneys, and Advocates Need to Know“. In it, I used 4 very different scenarios to illustrate the importance of comprehensive language evaluations for children with subtle language and learning needs. Today I would like to expound more on that post in order to explain, what actually constitutes a good independent comprehensive assessment. Continue reading What Makes an Independent Speech-Language-Literacy Evaluation a GOOD Evaluation?
Back to School SLP Efficiency Bundles™
 September is practically here and many speech language pathologists (SLPs) are looking to efficiently prepare for assessing and treating a variety of clients on their caseloads.
September is practically here and many speech language pathologists (SLPs) are looking to efficiently prepare for assessing and treating a variety of clients on their caseloads.
With that in mind, a few years ago I created SLP Efficiency Bundles™, which are materials highly useful for SLPs working with pediatric clients. These materials are organized by areas of focus for efficient and effective screening, assessment, and treatment of speech and language disorders.
A. General Assessment and Treatment Start-Up Bundle contains 5 downloads for general speech language assessment and treatment planning and includes:
- Speech Language Assessment Checklist for a Preschool Child
- Speech Language Assessment Checklist for a School-Aged Child
- Creating a Functional Therapy Plan: Therapy Goals & SOAP Note Documentation
- Selecting Clinical Materials for Pediatric Therapy
- Types and Levels of Cues and Prompts in Speech Language Therapy
B. The Checklists Bundle contains 7 checklists relevant to screening and assessment in speech language pathology
- Speech Language Assessment Checklist for a Preschool Child 3:00-6:11 years of age
- Speech Language Assessment Checklist for a School-Aged Child 7:00-11:11 years of age
- Speech Language Assessment Checklist for Adolescents 12-18 years of age
- Language Processing Deficits (LPD) Checklist for School Aged Children 7:00-11:11 years of age
- Language Processing Deficits (LPD) Checklist for Preschool Children 3:00-6:11 years of age
- Social Pragmatic Deficits Checklist for School Aged Children 7:00-11:11 years of age
- Social Pragmatic Deficits Checklist for Preschool Children 3:00-6:11 years of age
C. Social Pragmatic Assessment and Treatment Bundle contains 6 downloads for social pragmatic assessment and treatment planning (from 18 months through school age) and includes:
- Recognizing the Warning Signs of Social Emotional Difficulties in Language Impaired Toddlers and Preschoolers
- Behavior Management Strategies for Speech Language Pathologists
- Social Pragmatic Deficits Checklist for School Aged Children
- Social Pragmatic Deficits Checklist for Preschool Children
- Assessing Social Pragmatic Skills of School Aged Children
- Treatment of Social Pragmatic Deficits in School Aged Children
D. Multicultural Assessment and Treatment Bundle contains 2 downloads relevant to assessment and treatment of bilingual/multicultural children
- Language Difference vs. Language Disorder: Assessment & Intervention Strategies for SLPs Working with Bilingual Children
- Impact of Cultural and Linguistic Variables On Speech-Language Services
E. Narrative Assessment Bundle contains 3 downloads relevant to narrative assessment
- Narrative Assessments of Preschool and School Aged Children
- Understanding Complex Sentences
- Vocabulary Development: Working with Disadvantaged Populations
F. Fetal Alcohol Spectrum Disorders Assessment and Treatment Bundle contains 3 downloads relevant to FASD assessment and treatment
- Orofacial Observations of At-Risk Children
- Fetal Alcohol Spectrum Disorder: An Overview of Deficits
- Speech Language Assessment and Treatment of Children With Alcohol Related Disorders
G. Psychiatric Disorders Bundle contains 7 downloads relevant to language assessment and treatment in psychiatrically impaired children
- Recognizing the Warning Signs of Social Emotional Difficulties in Language Impaired Toddlers and Preschoolers
- Social Pragmatic Deficits Checklist for School Aged Children
- Social Pragmatic Deficits Checklist for Preschool Children
- Assessing Social Skills in Children with Psychiatric Disturbances
- Improving Social Skills of Children with Psychiatric Disturbances
- Behavior Management Strategies for Speech Language Pathologists
- Differential Diagnosis Of ADHD In Speech Language Pathology
You can find these bundles on SALE in my online store by clicking on the individual bundle links above. You can also purchase these products individually in my online store by clicking HERE.

Early Intervention Evaluations PART II: Assessing Suspected Motor Speech Disorders in Children Under 3
In my previous post on this topic, I brought up concerns regarding the paucity of useful information in EI SLP reports for children under 3 years of age and made some constructive suggestions of how that could be rectified. In 2013, I had written about another significant concern, which involved neurodevelopmental pediatricians (rather than SLPs), diagnosing Childhood Apraxia of Speech (CAS), without the adequate level of training and knowledge regarding motor speech disorders. Today, I wanted to combine both topics and delve deeper into another area of EI SLP evaluations, namely, assessments of toddlers with suspected motor speech disorders.
Firstly, it is important to note that CAS is disturbingly overdiagnosed. A cursory review of both parent and professional social media forums quickly reveals that this diagnosis is doled out like candy by both SLPs and medical professionals alike, often without much training and knowledge regarding the disorder in question. The child is under 3, has a limited verbal output coupled with a number of phonological processes, and the next thing you know, s/he is labeled as having Childhood Apraxia of Speech (CAS). But is this diagnosis truly that straightforward?
Let us begin with the fact that all reputable organizations involved in the dissemination of information on the topic of CAS (e.g., ASHA, CASANA, etc.), strongly discourage the diagnosis of CAS in children under three years of age with limited verbal output, and limited time spent in EBP therapy specifically targeting the remediation of motor speech disorders.
 Assessment of motor speech disorders in young children requires solid knowledge and expertise. That is because CAS has a number of overlapping symptoms with other speech sound disorders (e.g., severe phonological disorder, dysarthria, etc). Furthermore, symptoms which may initially appear as CAS may change during the course of intervention by the time the child is older (e.g., 3 years of age) which is why diagnosing toddlers under 3 years of age is very problematic and the use of “suspected” or “working” diagnosis is recommended (Davis & Velleman, 2000) in order to avoid misdiagnosis. Finally, the diagnosis of CAS is also problematic due to the fact that there are still to this day no valid or reliable standardized assessments sensitive to CAS detection (McCauley & Strand, 2008).
Assessment of motor speech disorders in young children requires solid knowledge and expertise. That is because CAS has a number of overlapping symptoms with other speech sound disorders (e.g., severe phonological disorder, dysarthria, etc). Furthermore, symptoms which may initially appear as CAS may change during the course of intervention by the time the child is older (e.g., 3 years of age) which is why diagnosing toddlers under 3 years of age is very problematic and the use of “suspected” or “working” diagnosis is recommended (Davis & Velleman, 2000) in order to avoid misdiagnosis. Finally, the diagnosis of CAS is also problematic due to the fact that there are still to this day no valid or reliable standardized assessments sensitive to CAS detection (McCauley & Strand, 2008).
In March 2017, Dr. Edythe Strand wrote an excellent article for the ASHA Leader entitled: “Appraising Apraxia“, in which she used a case study of a 3-year-old boy to describe how a differential diagnosis for CAS can be performed. She reviewed CAS characteristics, informal assessment protocols, aspects of diagnosis and treatment, and even included ‘Examples of Diagnostic Statements for CAS’ (which illustrate how clinicians can formulate their impressions regarding the child’s strengths and needs without explicitly labeling the child’s diagnosis as CAS).
Today, I’d like to share what information I tend to include in speech-language reports geared towards the assessing motor speech disorders in children under 3 years of age. I have a specific former client in mind for whom a differential diagnosis was particularly needed. Here’s why.
This particular 30-month client, TQ, (I did mention that I get quite a few clients for assessment around that age), was brought in due to parental concerns over her significantly reduced speech and expressive language abilities characterized by unintelligible “babbling-like” utterances and lack of expressive language. All of TQ’s developmental milestones with the exception of speech and language had been achieved grossly at age expectancy. She began limitedly producing word approximations at ~16 months of age but at 30 months of age, her verbal output was still very restricted. She mainly communicated via gestures, pointing, word approximations, and a handful of signs.
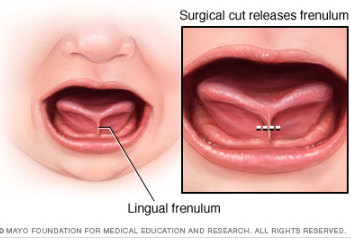
Interestingly, as an infant, she had a restricted lingual frenulum. However, since it did not affect her ability to feed, no surgical intervention was needed. Indeed, TQ presented with an adequate lingual movement for both feeding and speech sound production, so her ankyloglossia (or anterior tongue tie) was definitely not the culprit which caused her to have limited speech production.
 Prior to being reevaluated by me, TQ underwent an early intervention assessment at ~26 months of age. She was diagnosed with CAS by an evaluating SLP and was found to be eligible for speech-language services, which she began receiving shortly thereafter. However, Mrs. Q noted that TQ was making very few gains in therapy and her treating SLP was uncertain regarding why her progress in therapy was so limited. Mrs. Q was also rather uncertain that TQ’s diagnosis of CAS was indeed a correct one, which was another reason why she sought a second opinion.
Prior to being reevaluated by me, TQ underwent an early intervention assessment at ~26 months of age. She was diagnosed with CAS by an evaluating SLP and was found to be eligible for speech-language services, which she began receiving shortly thereafter. However, Mrs. Q noted that TQ was making very few gains in therapy and her treating SLP was uncertain regarding why her progress in therapy was so limited. Mrs. Q was also rather uncertain that TQ’s diagnosis of CAS was indeed a correct one, which was another reason why she sought a second opinion.
Assessment of TQ’s social-emotional functioning, play skills, and receptive language (via a combination of Revised Westby Play Scale (Westby, 2000), REEL-3, & PLS-5) quickly revealed that she was a very bright little girl who was developing on target in all of the tested areas. Assessment of TQ’s expressive language (via REEL-3, PLS-5 & LUI*), revealed profoundly impaired, expressive language abilities. But due to which cause?
Despite lacking verbal speech, TQ’s communicative frequency (how often she attempted to spontaneously and appropriately initiate interactions with others), as well as her communicative intent (e.g., gaining attention, making requests, indicating protests, etc), were judged to be appropriate for her age. She was highly receptive to language stimulation given tangible reinforcements and as the assessment progressed she was observed to significantly increase the number and variety of vocalizations and word approximations including delayed imitation of words and sounds containing bilabial and alveolar nasal phonemes.
For the purpose of TQ’s speech assessment, I was interested in gaining knowledge regarding the following:
- Automatic vs. volitional control
- Simple vs. complex speech production
- Consistency of productions on repetitions of the same words/word approximations
- Vowel Productions
- Imitation abilities
- Prosody
- Phonetic inventory
- Phonotactic Constraints
- Stimulability
 TQ’s oral peripheral examination yielded no difficulties with oral movements during non-speaking as well as speaking tasks. She was able to blow bubbles, stick out tongue, smile, etc as well as spontaneously vocalize without any difficulties. Her voice quality, pitch, loudness, and resonance during vocalizations and approximated utterances were judged to be appropriate for age and gender. Her prosody and fluency could not be determined due to lack of spontaneously produced continuous verbal output.
TQ’s oral peripheral examination yielded no difficulties with oral movements during non-speaking as well as speaking tasks. She was able to blow bubbles, stick out tongue, smile, etc as well as spontaneously vocalize without any difficulties. Her voice quality, pitch, loudness, and resonance during vocalizations and approximated utterances were judged to be appropriate for age and gender. Her prosody and fluency could not be determined due to lack of spontaneously produced continuous verbal output.
- Phonetic inventory of all the sounds TQ produced during the assessment is as follows:
- Consonants: plosive nasals (/m/) and alveolars (/t/, /d/, n), as well as a glide (/w/)
- Vowels: (/a/, /e/, /i/, /o/)
- TQ’s phonotactic repertoire was primarily comprised of word approximations restricted to specific sounds and consisted of CV (e.g., ne), VCV (e.g., ada), CVC (e.g., nyam), CVCV (e.g., nada), VCVC (e.g., adat), CVCVCV (nadadi), VCVCV(e.g., adada) syllable shapes
- TQ’s speech intelligibility in known and unknown contexts was profoundly reduced to unfamiliar listeners. However, her word approximations were consistent across all productions.
- Due to the above I could not perform an in-depth phonological processes analysis
However, by this time I had already formulated a working hypothesis regarding TQ’s speech production difficulties. Based on her speech sound assessment TQ presented with severe phonological disorder characterized by restricted sound inventory, simplification of sound sequences, as well as patterns of sound use errors (e.g., predominance of alveolar /d/ and nasal /n/ sounds when attempting to produce most word approximations) in speech (Stoel-Gammon, 1987).
TQ’s difficulties were not consistent with the diagnosis Childhood Apraxia of Speech (CAS) at that time due to the following:
- Adequate and varied production of vowels
- Lack of restricted use of syllables during verbalizations (TQ was observed to make verbalizations up to 3 syllables in length)
- Lack of disruptions in rate, rhythm, and stress of speech
- Frequent and spontaneous use of consistently produced verbalizations
- Lack of verbal groping behaviors when producing word-approximations
- Good control of pitch, loudness and vocal quality during vocalizations
 I felt that the diagnosis of CAS was not applicable because TQ lacked a verbal lexicon and no specific phonological intervention techniques had been trialed with her during the course of her brief therapy (~4 months) to elicit word productions (Davis & Velleman, 2000; Strand, 2003). While her EI speech therapist documented that therapy has primarily focused on ‘oral motor activities to increase TQ’s awareness of her articulators and to increase imitation of oral motor movements’, I knew that until a variety of phonological/motor-speech specific interventions had been trialed over a period of time (at least ~6 months as per Davis & Velleman, 2000) the diagnosis of CAS could not be reliably made.
I felt that the diagnosis of CAS was not applicable because TQ lacked a verbal lexicon and no specific phonological intervention techniques had been trialed with her during the course of her brief therapy (~4 months) to elicit word productions (Davis & Velleman, 2000; Strand, 2003). While her EI speech therapist documented that therapy has primarily focused on ‘oral motor activities to increase TQ’s awareness of her articulators and to increase imitation of oral motor movements’, I knew that until a variety of phonological/motor-speech specific interventions had been trialed over a period of time (at least ~6 months as per Davis & Velleman, 2000) the diagnosis of CAS could not be reliably made.
I still, however, wanted to be cautious as there were a few red flags I had noted which may have potentially indicative of a non-CAS motor speech involvement, due to which I wanted to include some recommendations pertaining to motor speech remediation.
Now it is possible that after 6 months of intensive application of EBP phonological and motor speech approaches TQ would have turned 3 and still presented with highly restricted speech sound inventory and profoundly impaired speech production, making her eligible for the diagnosis of CAS in earnest. However, at the time of my assessment, making such diagnosis in view of all the available evidence would have been both clinically inappropriate and unethical.
So what were my recommendations you may ask? Well, I provisionally diagnosed TQ with a severe phonological disorder and recommended that among a variety of phonologically-based approaches to trial, an EBP approach to the treatment of motor speech disorders be also used with her for a period of 6 months to determine if it would expedite speech gains.
 *For those of you who are interested in the latest EBP treatment for motor speech disorders, current evidence supports the use of the Rapid Syllable Transition Treatment (ReST). ReST is a free EBP treatment developed by the SLPs at the University of Sydney, which uses nonsense words, designed to help children coordinate movements across syllables in long words and phrases as well as helps them learn new speech movements. It is, however, important to note for young children with highly restricted sound inventories, characterized by a lack of syllable production, ReST will not be applicable. For them, the Integral Stimulation/Dynamic Temporal and Tactile Cueing (DTTC) approaches do have some limited empirical support.
*For those of you who are interested in the latest EBP treatment for motor speech disorders, current evidence supports the use of the Rapid Syllable Transition Treatment (ReST). ReST is a free EBP treatment developed by the SLPs at the University of Sydney, which uses nonsense words, designed to help children coordinate movements across syllables in long words and phrases as well as helps them learn new speech movements. It is, however, important to note for young children with highly restricted sound inventories, characterized by a lack of syllable production, ReST will not be applicable. For them, the Integral Stimulation/Dynamic Temporal and Tactile Cueing (DTTC) approaches do have some limited empirical support.
I also made sure to make a note in my report regarding the inappropriate use of non-speech oral motor exercises (NSOMEs) in therapy, indicating that there is NO research to support the use of NSOMEs to stimulate speech production (Lof, 2010).
In addition to the trialing of phonological and motor based approaches I also emphasized the need to establish consistent lexicon via development of functional words needed in daily communication and listed a number of examples across several categories. I made recommendations regarding select approaches and treatment techniques to trial in therapy, as well as suggestions for expansion of sounds and structures. Finally, I made suggestions for long and short term therapy goals for a period of 6 months to trial with TQ in therapy and provided relevant references to support the claims I’ve made in my report.
You may be interested in knowing that nowadays TQ is doing quite well, and at this juncture, she is still, ineligible for the diagnosis CAS (although she needs careful ongoing monitoring with respect to the development of reading difficulties when she is older).
 Now I know that some clinicians will be quick to ask me: “What’s the harm in overdiagnosing CAS if the child’s speech production will still be treated via the application of motor speech production principles?” Well, aside from the fact that it’s obviously unethical and can result in terrifying the parents into obtaining all sorts of questionable and even downright harmful bunk treatments for their children, the treatment may only be limitedly appropriate, and may not result in the best possible outcomes for a particular child. To illustrate, TQ never presented with CAS and as such, while she may have initially limitedly benefited from the application of motor speech principles to address her speech production, shortly thereafter, the application of the principles of the dynamic systems theory is what brought about significant changes in her phonological repertoire.
Now I know that some clinicians will be quick to ask me: “What’s the harm in overdiagnosing CAS if the child’s speech production will still be treated via the application of motor speech production principles?” Well, aside from the fact that it’s obviously unethical and can result in terrifying the parents into obtaining all sorts of questionable and even downright harmful bunk treatments for their children, the treatment may only be limitedly appropriate, and may not result in the best possible outcomes for a particular child. To illustrate, TQ never presented with CAS and as such, while she may have initially limitedly benefited from the application of motor speech principles to address her speech production, shortly thereafter, the application of the principles of the dynamic systems theory is what brought about significant changes in her phonological repertoire.
That is why the correct diagnosis is so important for young children under 3 years of age. But before it can be made, extensive (reputable and evidence supported) training and education are needed by evaluating SLPs on the assessment and treatment of motor speech disorders in young children.
References:
- Davis, B & Velleman, S (2000). Differential diagnosis and treatment of developmental apraxia of speech in infants and toddlers”. The Transdisciplinary Journal. 10 (3): 177 – 192.
- Lof, G., & Watson, M. (2010). Five reasons why nonspeech oral-motor exercises do not work. Perspectives on School-Based Issues, 11.109-117.
- McCauley RJ, Strand EA. (2008). A Review of Standardized Tests of Nonverbal Oral and Speech Motor Performance in Children. American Journal of Speech-Language Pathology, 17,81-91.
- McCauley R.J., Strand E., Lof, G.L., Schooling T. & Frymark, T. (2009). Evidence-Based Systematic Review: Effects of Nonspeech Oral Motor Exercises on Speech, American Journal of Speech-Language Pathology, 18, 343-360.
- Murray, E., McCabe, P. & Ballard, K.J. (2015). A Randomized Control Trial of Treatments for Childhood Apraxia of Speech. Journal of Speech, Language and Hearing Research 58 (3) 669-686.
- Stoel-Gammon, C. (1987). Phonological skills of 2-year-olds. Language, Speech, and Hearing Services in Schools, 18, 323-329.
- Strand, E (2003). Childhood apraxia of speech: suggested diagnostic markers for the young child. In Shriberg, L & Campbell, T (Eds) Proceedings of the 2002 childhood apraxia of speech research symposium. Carlsbad, CA: Hendrix Foundation.
- Strand, E, McCauley, R, Weigand, S, Stoeckel, R & Baas, B (2013) A Motor Speech Assessment for Children with Severe Speech Disorders: Reliability and Validity Evidence. Journal of Speech Language and Hearing Research, vol 56; 505-520.
Treatment of Children with “APD”: What SLPs Need to Know
 In recent years there has been an increase in research on the subject of diagnosis and treatment of Auditory Processing Disorders (APD), formerly known as Central Auditory Processing Disorders or CAPD.
In recent years there has been an increase in research on the subject of diagnosis and treatment of Auditory Processing Disorders (APD), formerly known as Central Auditory Processing Disorders or CAPD.
More and more studies in the fields of audiology and speech-language pathology began confirming the lack of validity of APD as a standalone (or useful) diagnosis. To illustrate, in June 2015, the American Journal of Audiology published an article by David DeBonis entitled: “It Is Time to Rethink Central Auditory Processing Disorder Protocols for School-Aged Children.” In this article, DeBonis pointed out numerous inconsistencies involved in APD testing and concluded that “routine use of APD test protocols cannot be supported” and that [APD] “intervention needs to be contextualized and functional” (DeBonis, 2015, p. 124) Continue reading Treatment of Children with “APD”: What SLPs Need to Know
The End of See it, Zap it! Ankyloglossia (Tongue-Tie) Controversies in Research and Clinical Practice
 Today it is my pleasure and privilege to interview 3 Australian lactation consultations: Lois Wattis, Renee Kam, and Pamela Douglas, the authors of a March 2017 article in the Breastfeeding Review: “Three experienced lactation consultants reflect upon the oral tie phenomenon” (which can be found HERE).
Today it is my pleasure and privilege to interview 3 Australian lactation consultations: Lois Wattis, Renee Kam, and Pamela Douglas, the authors of a March 2017 article in the Breastfeeding Review: “Three experienced lactation consultants reflect upon the oral tie phenomenon” (which can be found HERE).
Tatyana Elleseff: Colleagues, as you very well know, the subject of ankyloglossia or tongue tie affecting breastfeeding and speech production has risen into significant prominence in the past several years. Numerous journal articles, blog posts, as well as social media forums have been discussing this phenomenon with rather conflicting recommendations. Many health professionals and parents are convinced that “releasing the tie” or performing either a frenotomy or frenectomy will lead to significant improvements in speech and feeding.
 Presently, systematic reviews1-3 demonstrate there is insufficient evidence for the above. However, when many professionals including myself, cite reputable research explaining the lack of support of surgical intervention for tongue tie, there has been a pushback on the part of a number of other health professionals including lactation consultants, nurses, dentists, as well as speech-language pathologists stating that in their clinical experience surgical intervention does resolve issues with tongue tie as related to speech and feeding.
Presently, systematic reviews1-3 demonstrate there is insufficient evidence for the above. However, when many professionals including myself, cite reputable research explaining the lack of support of surgical intervention for tongue tie, there has been a pushback on the part of a number of other health professionals including lactation consultants, nurses, dentists, as well as speech-language pathologists stating that in their clinical experience surgical intervention does resolve issues with tongue tie as related to speech and feeding.
So today, given your 33 combined years of practice as lactation consultants I would love to ask your some questions regarding the tongue tie phenomena.
I would like to begin our discussion with a description of normal breastfeeding and what can interfere with it from an anatomical and physiological standpoint for mothers and babies.
 Now, many of this blog’s readers already know that a tongue tie occurs when the connective tissue under the tongue known as a lingual frenulum restricts tongue movement to some degree and adversely affects its function. But many may not realize that children can present with a normal anatomical variant of “ties” which can be completely asymptomatic. Can you please address that?
Now, many of this blog’s readers already know that a tongue tie occurs when the connective tissue under the tongue known as a lingual frenulum restricts tongue movement to some degree and adversely affects its function. But many may not realize that children can present with a normal anatomical variant of “ties” which can be completely asymptomatic. Can you please address that?
Lois Wattis: “Normal” breastfeeding takes time and skill to achieve. The breastfeeding dyad is multifactorial, influenced by maternal breast and nipple anatomy combined with the infant’s facial and oral structures, all of which are highly variable. Mothers who have successfully breastfed the first baby may encounter problems with subsequent babies due to size (e.g., smaller, larger, etc.), be compromised by birth interventions or drugs during labor, or incur birth injuries – all of which can affect the initiation of breastfeeding and progression to a happy and comfortable feeding relationship. Unfortunately, the overview of each dyad’s story can be lost when tunnel vision of either health provider or parents regarding the baby’s oral anatomy is believed to be the chief influencer of breastfeeding success or failure.
Tatyana Elleseff: Colleagues, what do we know regarding the true prevalence of various ‘tongue ties’? Are there any studies of good quality?
 Pamela Douglas: In a literature review in 2005, Hall and Renfrew acknowledged that the true prevalence of ankyloglossia remained unknown, though they estimated 3-4% of newborns.4
Pamela Douglas: In a literature review in 2005, Hall and Renfrew acknowledged that the true prevalence of ankyloglossia remained unknown, though they estimated 3-4% of newborns.4
After 2005, once the diagnosis of posterior tongue-tie (PTT) had been introduced,5, 6 attempts to quantify incidence of tongue-tie have remained of very poor quality, but estimates currently rest at between 4-10%.7
The problem is that there is a lack of definitional clarity concerning the diagnosis of PTT. Consequently, anterior or classic tongue tie CTT is now often conflated with PTT simply as ‘tongue-tie’ (TT).
Tatyana Elleseff: Thank you for clarifying it. In addition to the anterior and posterior tongue tie labels, many parents and professionals also frequently hear the terms lip tie and buccal ties. Is there’s reputable research behind these terms indicating that these ties can truly impact speech and feeding?
Pamela Douglas: Current definitions of ankyloglossia tend to confuse oral and tongue function (which is affected by multiple variables, and in particular by a fit and hold in breastfeeding) with structure (which is highly anatomically variable for both the tongue length and appearance and lingual and maxillary frenula).
For my own purposes, I define CTT as Type 1 and 2 on the Coryllos-Genna-Watson scale.8 In clinical practice, I also find it useful to rate the anterior membrane by the percentage of the undersurface of the tongue into which the membrane connects, applying the first two categories of the Griffiths Classification System.9
There is a wide spectrum of lingual frenula morphologies and elasticities, and deciding where to draw a line between a normal variant and CTT will depend on the clinical judgment concerning the infant’s capacity for pain-free efficient milk transfer. However, that means we need to have an approach to fit and hold that we are confident does optimize pain-free efficient milk transfer and at the moment, research shows that not only do the old ‘hands on’ approach to fit and hold not work, but that baby-led attachment is also not enough for many women. This is why at the Possums Clinic we’ve been working on developing an approach to fit and hold (gestalt breastfeeding) that builds on baby-led attachment but also integrates the findings of the latest ultrasound studies.
I personally don’t find the diagnoses of posterior tongue tie PTT and upper lip tie ULT helpful, and don’t use them. Lois, Renee and myself find that a wide spectrum of normal anatomic lingual and maxillary frenula variants are currently being misdiagnosed as a PTT and ULT, which has worried us and led Lois to initiate the article with Renee.
Tatyana Elleseff: Segueing from the above question: is there an established criterion based upon which a decision is made by relevant professionals to “release” the tie and if so can you explain how it’s determined?
 Lois Wattis: When an anterior frenulum is attached at the tongue tip or nearby and is short enough to cause restriction of lift towards the palate, usually associated with extreme discomfort for the breastfeeding mother, I have no reservations about snipping it to release the tongue to enable optimal function for breastfeeding. If a simple frenotomy is going to assist the baby to breastfeed well it is worth doing, and as soon as possible. What I do encounter in my clinical practice are distressed and disempowered mothers whose baby has been labeled as having a posterior tongue tie and/or upper lip tie which is the cause of current and even future problems. Upon examination, the baby has completely normal oral anatomy and breastfeeding upskilling and confidence building of both mother and baby enables the dyad to go forward with strategies which address all elements of their unique story.
Lois Wattis: When an anterior frenulum is attached at the tongue tip or nearby and is short enough to cause restriction of lift towards the palate, usually associated with extreme discomfort for the breastfeeding mother, I have no reservations about snipping it to release the tongue to enable optimal function for breastfeeding. If a simple frenotomy is going to assist the baby to breastfeed well it is worth doing, and as soon as possible. What I do encounter in my clinical practice are distressed and disempowered mothers whose baby has been labeled as having a posterior tongue tie and/or upper lip tie which is the cause of current and even future problems. Upon examination, the baby has completely normal oral anatomy and breastfeeding upskilling and confidence building of both mother and baby enables the dyad to go forward with strategies which address all elements of their unique story.
Although the Hazelbaker Assessment Tool for Lingual Frenulum Function (ATLFF) is a pioneering contribution, bringing us our first systematized approach to examination of the infant’s tongue and oral connective tissues, it is unreliable as a tool for decision-making concerning frenotomy.10-12 In practice many of the item criteria are highly subjective. Although one study found moderate inter-rater reliability on the ATLFF’s structural items, the authors did not find inter-rater reliability on most of the functional items.13 In my clinical experience, there is no reliable correlation between what the tongue is observed to do during oral examinations and what occurs during breastfeeding, other than in the case of classic tongue-tie (excluding congenital craniofacial abnormalities from this discussion.
In my practice as a Lactation Consultant in an acute hospital setting I use a combination of the available assessment tools mainly for documentation purposes, however, the most important tools I use are my eyes and my ears. Observing the mother and baby physical combination and interactions, and suggesting adjustments where indicated to the positioning and attachment technique used (which Pam calls fit and hold) can very often resolve difficulties immediately – even if the baby also has an obvious frenulum under his/her tongue. Listening to the mother’s feedback, and observing the baby’s responses are primary indicators of whether further intervention is needed, or not. Watching how the baby achieves and retains the latch is key, then the examination of baby’s mouth to assess tongue mobility and appearance provide final information about whether baby’s ability to breastfeed comfortably is or is not being hindered by a restrictive lingual frenulum.
Tatyana Elleseff: So frenotomy is an incision (cut) of lingual frenum while frenectomy (complete removal) is an excision of lingual frenum. Both can be performed via various methods of “release”. What effects on breastfeeding have you seen with respect to healing?
Lois Wattis: The significant difference between both procedures involves the degree of invasiveness and level of pain experienced during and after the procedures, and the differing time it takes for the resumption and/or improvement in breastfeeding comfort and efficacy.
It is commonplace for a baby who has had a simple incision to breastfeed immediately after the procedure and exhibit no further signs of discomfort or oral aversion. Conversely, the baby who has had laser division(s) may breastfeed soon after the procedure while topical anesthetics are still working. However, many infants demonstrate discomfort, extreme pain responses and reluctance to feed for days or weeks following a laser treatment. Parents are warned to expect delays resuming feeding and the baby is usually also subjected to wound “stretches” for weeks following the laser treatments. Unfortunately, in my clinical practice I see many parents and babies who are very traumatized by this whole process, and in many cases, breastfeeding can be derailed either temporarily or permanently.
 Tatyana Elleseff: Thank you! This is highly relevant information for both health professionals and parents alike. I truly appreciate your clinical expertise on this topic. While we are on the topic of restrictive lingual frenulums can we discuss several recent articles published on surgical interventions for the above? For example (Ghaheri, Cole, Fausel, Chuop & Mace, 2016), recently published the result of their study which concluded that: “Surgical release of tongue-tie/lip-tie results in significant improvement in breastfeeding outcomes”. Can you elucidate upon the study design and its findings?
Tatyana Elleseff: Thank you! This is highly relevant information for both health professionals and parents alike. I truly appreciate your clinical expertise on this topic. While we are on the topic of restrictive lingual frenulums can we discuss several recent articles published on surgical interventions for the above? For example (Ghaheri, Cole, Fausel, Chuop & Mace, 2016), recently published the result of their study which concluded that: “Surgical release of tongue-tie/lip-tie results in significant improvement in breastfeeding outcomes”. Can you elucidate upon the study design and its findings?
Pamela Douglas: Pre-post surveys, such as Ghaheri et al’s 2016 study, are notoriously methodologically weak and prone to interpretive bias.14
Renee Kam: Research about the efficacy of releasing ULTs to improve breastfeeding outcomes is seriously lacking. There is no reliable assessment tool for upper lip-tie and a lack of evidence to support the efficacy of a frenotomy of labial frenula in breastfed babies. The few studies which have included ULT release have either included very small numbers of babies having upper lip-tie releases or have included babies having a release upper lip ties and tongue ties at the same time, making it impossible to know if any improvements were due to the tongue-tie release, upper lip-tie release or both. Here, to answer your previous question, to date, no research has looked into the treatment of buccal ties for breastfeeding outcomes.
There are various classification scales for labial frenulums such as the Kotlow scale. The title of this scale is misleading as it contains the word ‘tie’. Hence it can give some people the incorrect assumption that a class III or IV labial frenulum is somehow a problem. What this scale actually shows is the normal range of insertion sites for a labial frenulum. And, in normal cases, the vast majority of babies’ labial frenulums insert low down on the upper gum (class III) or even wrap around it (class IV). It’s important to note that, for effective breastfeeding, the upper lip does not have to flange out in order to create a seal. It just has to rest in a neutral position — not flanged out, not tucked in.
Lois Wattis: I entirely agree with Renee’s view about the neutrality of the upper lip, including the labial frenulum, in relation to latch for breastfeeding. Even babies with asymmetrical facial features, cleft lips and other permanent and temporary anomalies only need to achieve a seal with the upper lip to breastfeed successfully.
 Tatyana Elleseff: Thank you for that. In addition to studies on tongue tie revisions and breastfeeding outcomes, there has been an increase in studies, specifically Kotlow (2016) and Siegel (2016), which claimed that surgical intervention improves outcomes for acid reflux and aerophagia in babies”. Can you discuss these studies design and findings?
Tatyana Elleseff: Thank you for that. In addition to studies on tongue tie revisions and breastfeeding outcomes, there has been an increase in studies, specifically Kotlow (2016) and Siegel (2016), which claimed that surgical intervention improves outcomes for acid reflux and aerophagia in babies”. Can you discuss these studies design and findings?
Renee Kam: The AIR hypothesis has led to reflux being used as another reason to diagnose the oral anatomic abnormalities in infants in the presence of breastfeeding problems. More research with objective indicators and less vested interest is needed in this area. A thorough understanding of normal infant behavior and feeding problems which aren’t tie related are also imperative before any conclusions about AIR can be reached.
Tatyana Elleseff: One final question, colleagues are you aware of any studies which describe long-term outcomes of surgical interventions for tongue ties?
Pamela Douglas: The systematic reviews note that there is a lack of evidence demonstrating long-term outcomes of surgical interventions.
Tatyana Elleseff: Thank you for such informative discussion, colleagues.
 There you have it, readers. Both research and clinical practice align to indicate that:
There you have it, readers. Both research and clinical practice align to indicate that:
- There’s significant normal variation when it comes to most anatomical structures including the frenulum
- Just because a child presents with restricted frenulum does not automatically imply adverse feeding as well as speech outcomes and immediately necessitates a tongue tie release
- When breastfeeding difficulties arise, in the presence of restricted frenulum, it is very important to involve an experienced lactation specialist who will perform a differential diagnosis in order to determine the source of the baby’s true breastfeeding difficulties
Now, I’d like to take a moment and address the myth of tongue ties affecting speech production, which continues to persist among speech-language pathologists despite overwhelming evidence to the contrary.
For that purpose, I will use excerpts from an excellent ASHA Leader December 2005 article written by an esteemed Dr. Kummer who is certainly well qualified to discuss this issue. According to Dr. Kummer, “there is no empirical evidence in the literature that ankyloglossia typically causes speech defects. On the contrary, several authors, even from decades ago, have disputed the belief that there is a strong causal relationship (Wallace, 1963; Block, 1968; Catlin & De Haan, 1971; Wright, 1995; Agarwal & Raina, 2003).”
 Since many children with restricted frenulum do not have any speech production difficulties, Dr Kummer explains why that is the case by discussing the effect of tongue tip positioning for speech production.
Since many children with restricted frenulum do not have any speech production difficulties, Dr Kummer explains why that is the case by discussing the effect of tongue tip positioning for speech production.
“Lingual-alveolar sounds (t, d, n) are produced with the top of the tongue tip and therefore, they can be produced with very little tongue elevation or mobility.
The /s/ and /z/ sounds require the tongue tip to be elevated only slightly but can be produced with little distortion if the tip is down.
The most the tongue tip needs to elevate is to the alveolar ridge for the production of an /l/. However, this sound can actually be produced with the tongue tip down and the dorsum of the tongue up against the alveolar ridge. Even an /r/ sound can be produced with the tongue tip down as long as the back of the tongue is elevated on both sides.
The most the tongue needs to protrude is to the back of the maxillary incisors for the production of /th/. All of these sounds can usually be produced, even with significant tongue tip restriction. This can be tested by producing these sounds with the tongue tip pressed down or against the mandibular gingiva. This results in little, if any, distortion.” (Kummer, 2005, ASHA Leader)
In 2009, Dr. Sharynne McLeod, did research on electropalatography of speech sounds with adults. Her findings (below) which are coronal images of tongue positioning including bracing, lateral contact and groove formation for consonants support the above information provided by Dr. Kummer.
Once again research and clinical practice align to indicate that there’s insufficient evidence to indicate the effect of restricted frenulum on the production of speech sounds.
Finally, I would like to conclude this post with a list of links from recent systematic reviews summarizing the latest research on this topic.
Ankyloglossia/Tongue Tie Systematic Review Summaries to Date (2017):
- A small body of evidence suggests that frenotomy may be associated with mother reported improvements in breastfeeding, and potentially in nipple pain, but with small, short-term studies with inconsistent methodology, the strength of the evidence is low to insufficient.
- In an infant with tongue-tie and feeding difficulties, surgical release of the tongue-tie does not consistently improve infant feeding but is likely to improve maternal nipple pain. Further research is needed to clarify and confirm this effect.
- Data are currently insufficient for assessing the effects of frenotomy on nonbreastfeeding outcomes that may be associated with ankyloglossia
- Given the lack of good-quality studies and limitations in the measurement of outcomes, we considered the strength of the evidence for the effect of surgical interventions to improve speech and articulation to be insufficient.
- Large temporal increases and substantial spatial variations in ankyloglossia and frenotomy rates were observed that may indicate a diagnostic suspicion bias and increasing use of a potentially unnecessary surgical procedure among infants.
References
- Power R, Murphy J. Tongue-tie and frenotomy in infants with breastfeeding difficulties: achieving a balance. Archives of Disease in Childhood 2015;100:489-494.
- Francis DO, Krishnaswami S, McPheeters M. Treatment of ankyloglossia and breastfeeding outcomes: a systematic review. Pediatrics. 2015;135(6):e1467-e1474.
- O’Shea JE, Foster JP, O’Donnell CPF, Breathnach D, Jacobs SE, Todd DA, et al. Frenotomy for tongue-tie in newborn infants (Review). Cochrane Database of Systematic Reviews. 2017 (3):Art. No.:CD011065.
- Hall D, Renfrew M. Tongue tie. Archives of Disease in Childhood. 2005;90:1211-1215.
- Coryllos E, Watson Genna C, Salloum A. Congenital tongue-tie and its impact on breastfeeding. Breastfeeding: Best for Mother and Baby, American Academy of Pediatrics. 2004 Summer:1-6.
- Coryllos EV, Watson Genna C, LeVan Fram J. Minimally Invasive Treatment for Posterior Tongue-Tie (The Hidden Tongue-Tie). In: Watson Genna C, editor. Supporting Sucking Skills. Burlington, MA: Jones and Bartlett Learning; 2013. p. 243-251.
- National Health and Medical Research Council. Infant feeding guidelines: information for health workers. In: Government A, editor. 2012. p. https://www.nhmrc.gov.au/guidelines-publications/n56.
- Watson Genna C, editor. Supporting sucking skills in breastfeeding infants. Burlington, MA: Jones and Bartlett Learning; 2016.
- Griffiths DM. Do tongue ties affect breastfeeding? . Journal of Human Lactation. 2004;20:411.
- Ricke L, Baker N, Madlon-Kay D. Newborn tongue-tie: prevalence and effect on breastfeeding. Journal of American Board of Family Practice. 2005;8:1-8.
- Madlon-Kay D, Ricke L, Baker N, DeFor TA. Case series of 148 tongue-tied newborn babies evaluated with the assessment tool for lingual function. Midwifery. 2008;24:353-357.
- Ballard JL, Auer CE, Khoury JC. Ankyloglossia: assessment, incidence, and effect of frenuloplasty on the breastfeeding dyad. Pediatrics. 2002;110:e63.
- Amir L, James JP, Donath SM. Reliability of the Hazelbaker Assessment Tool for Lingual Frenulum Function. International Breastfeeding Journal. 2006;1:3.
- Douglas PS. Conclusions of Ghaheri’s study that laser surgery for posterior tongue and lip ties improve breastfeeding are not substantiated. Breastfeeding Medicine. 2017;12(3):DOI: 10.1089/bfm.2017.0008.
Author Bios (in alphabetical order):
 Dr. Pamela Douglas is the founder of a charitable organization, the Possums Clinic, a general practitioner since 1987, an IBCLC (1994-2004; 2012-Present) and researcher. She is an Associate Professor (Adjunct) with the Centre for Health Practice Innovation, Griffith University, and a Senior Lecturer with the Discipline of General Practice, The University of Queensland. Pam enjoys working clinically with families across the spectrum of challenges in early life, many complex (including breastfeeding difficulty) unsettled infant behaviors, reflux, allergies, tongue-tie/oral connective tissue problems, and gut problems. She is author of The discontented little baby book: all you need to know about feeds, sleep and crying (UQP) www.possumsonline.com; www.pameladouglas.com.au
Dr. Pamela Douglas is the founder of a charitable organization, the Possums Clinic, a general practitioner since 1987, an IBCLC (1994-2004; 2012-Present) and researcher. She is an Associate Professor (Adjunct) with the Centre for Health Practice Innovation, Griffith University, and a Senior Lecturer with the Discipline of General Practice, The University of Queensland. Pam enjoys working clinically with families across the spectrum of challenges in early life, many complex (including breastfeeding difficulty) unsettled infant behaviors, reflux, allergies, tongue-tie/oral connective tissue problems, and gut problems. She is author of The discontented little baby book: all you need to know about feeds, sleep and crying (UQP) www.possumsonline.com; www.pameladouglas.com.au
 Renee Kam qualified with a Bachelor of Physiotherapy from the University of Melbourne in 2000. She then worked as a physiotherapist for 6 years, predominantly in the areas of women’s health, pediatric and musculoskeletal physiotherapy. She became an Australian Breastfeeding Association Breastfeeding (ABA) counselor in 2010 and obtained the credential of International Board Certified Lactation Consultant (IBCLC) in 2012. In 2013, Renee’s book, The Newborn Baby Manual, was published which covers the topics that Renee is passionate about; breastfeeding, baby sleep and baby behavior. These days, Renee spends most of her time being a mother to her two young daughters, writing breastfeeding content for BellyBelly.com.au, fulfilling her role as national breastfeeding information manager with ABA and working as an IBCLC in private practice and at a private hospital in Melbourne, Australia.
Renee Kam qualified with a Bachelor of Physiotherapy from the University of Melbourne in 2000. She then worked as a physiotherapist for 6 years, predominantly in the areas of women’s health, pediatric and musculoskeletal physiotherapy. She became an Australian Breastfeeding Association Breastfeeding (ABA) counselor in 2010 and obtained the credential of International Board Certified Lactation Consultant (IBCLC) in 2012. In 2013, Renee’s book, The Newborn Baby Manual, was published which covers the topics that Renee is passionate about; breastfeeding, baby sleep and baby behavior. These days, Renee spends most of her time being a mother to her two young daughters, writing breastfeeding content for BellyBelly.com.au, fulfilling her role as national breastfeeding information manager with ABA and working as an IBCLC in private practice and at a private hospital in Melbourne, Australia.
 Lois Wattis is a Registered Nurse/Midwife, International Board Certified Lactation Consultant and Fellow of the Australian College of Midwives. Working in both hospital and community settings, Lois has enhanced her midwifery skills and expertise by providing women-centred care to thousands of mothers and babies, including more than 50 women who chose to give birth at home. Lois’ qualifications include Bachelor of Nursing Degree (Edith Cowan University, Perth WA), Post Graduate Diploma in Clinical Nursing, Midwifery (Curtin University, Perth WA), accreditation as Independent Practising Midwife by the Australian College of Midwives in 2002 and International Board Certified Lactation Consultant in 2004. Lois was inducted as a Fellow of the Australian College of Midwives (FACM) in 2005 in recognition of her services to women and midwifery in Australia. Lois has authored numerous articles which have been published internationally in parenting and midwifery journals, and shares her broad experience via her creations “New Baby 101” book, smartphone App, on-line videos and Facebook page. www.newbaby101.com.au Lois has worked for the past 10 years in Qld, Australia in a dedicated Lactation Consultant role as well as in private practice www.birthjourney.com
Lois Wattis is a Registered Nurse/Midwife, International Board Certified Lactation Consultant and Fellow of the Australian College of Midwives. Working in both hospital and community settings, Lois has enhanced her midwifery skills and expertise by providing women-centred care to thousands of mothers and babies, including more than 50 women who chose to give birth at home. Lois’ qualifications include Bachelor of Nursing Degree (Edith Cowan University, Perth WA), Post Graduate Diploma in Clinical Nursing, Midwifery (Curtin University, Perth WA), accreditation as Independent Practising Midwife by the Australian College of Midwives in 2002 and International Board Certified Lactation Consultant in 2004. Lois was inducted as a Fellow of the Australian College of Midwives (FACM) in 2005 in recognition of her services to women and midwifery in Australia. Lois has authored numerous articles which have been published internationally in parenting and midwifery journals, and shares her broad experience via her creations “New Baby 101” book, smartphone App, on-line videos and Facebook page. www.newbaby101.com.au Lois has worked for the past 10 years in Qld, Australia in a dedicated Lactation Consultant role as well as in private practice www.birthjourney.com
Is it a Difference or a Disorder? Free Resources for SLPs Working with Bilingual and Multicultural Children
 For bilingual and monolingual SLPs working with bilingual and multicultural children, the question of: “Is it a difference or a disorder?” arises on a daily basis as they attempt to navigate the myriad of difficulties they encounter in their attempts at appropriate diagnosis of speech, language, and literacy disorders.
For bilingual and monolingual SLPs working with bilingual and multicultural children, the question of: “Is it a difference or a disorder?” arises on a daily basis as they attempt to navigate the myriad of difficulties they encounter in their attempts at appropriate diagnosis of speech, language, and literacy disorders.
 For that purpose, I’ve recently created a Checklist for Identification of Speech-Language Disorders in Bilingual and Multicultural Children. Its aim is to assist Speech Language Pathologists (SLPs) and Teachers in the decision-making process of how to appropriately identify bilingual/multicultural children who present with speech-language delay/deficits (vs. a language difference), for the purpose of initiating a formal speech-language-literacy evaluation. The goal is to ensure that educational professionals are appropriately identifying bilingual children for assessment and service provision due to legitimate speech language deficits/concerns, and are not over-identifying students because they speak multiple languages or because they come from low socioeconomic backgrounds. It is very important to understand that true language impairment in bilingual children will be evident in both languages from early childhood onwards, and thus will adversely affect the learning of both languages.
For that purpose, I’ve recently created a Checklist for Identification of Speech-Language Disorders in Bilingual and Multicultural Children. Its aim is to assist Speech Language Pathologists (SLPs) and Teachers in the decision-making process of how to appropriately identify bilingual/multicultural children who present with speech-language delay/deficits (vs. a language difference), for the purpose of initiating a formal speech-language-literacy evaluation. The goal is to ensure that educational professionals are appropriately identifying bilingual children for assessment and service provision due to legitimate speech language deficits/concerns, and are not over-identifying students because they speak multiple languages or because they come from low socioeconomic backgrounds. It is very important to understand that true language impairment in bilingual children will be evident in both languages from early childhood onwards, and thus will adversely affect the learning of both languages.
However, today the aim of today’s post is not on the above product but rather on the FREE free bilingual and multicultural resources available to SLPs online in their quest of differentiating between a language difference from a language disorder in bilingual and multicultural children.
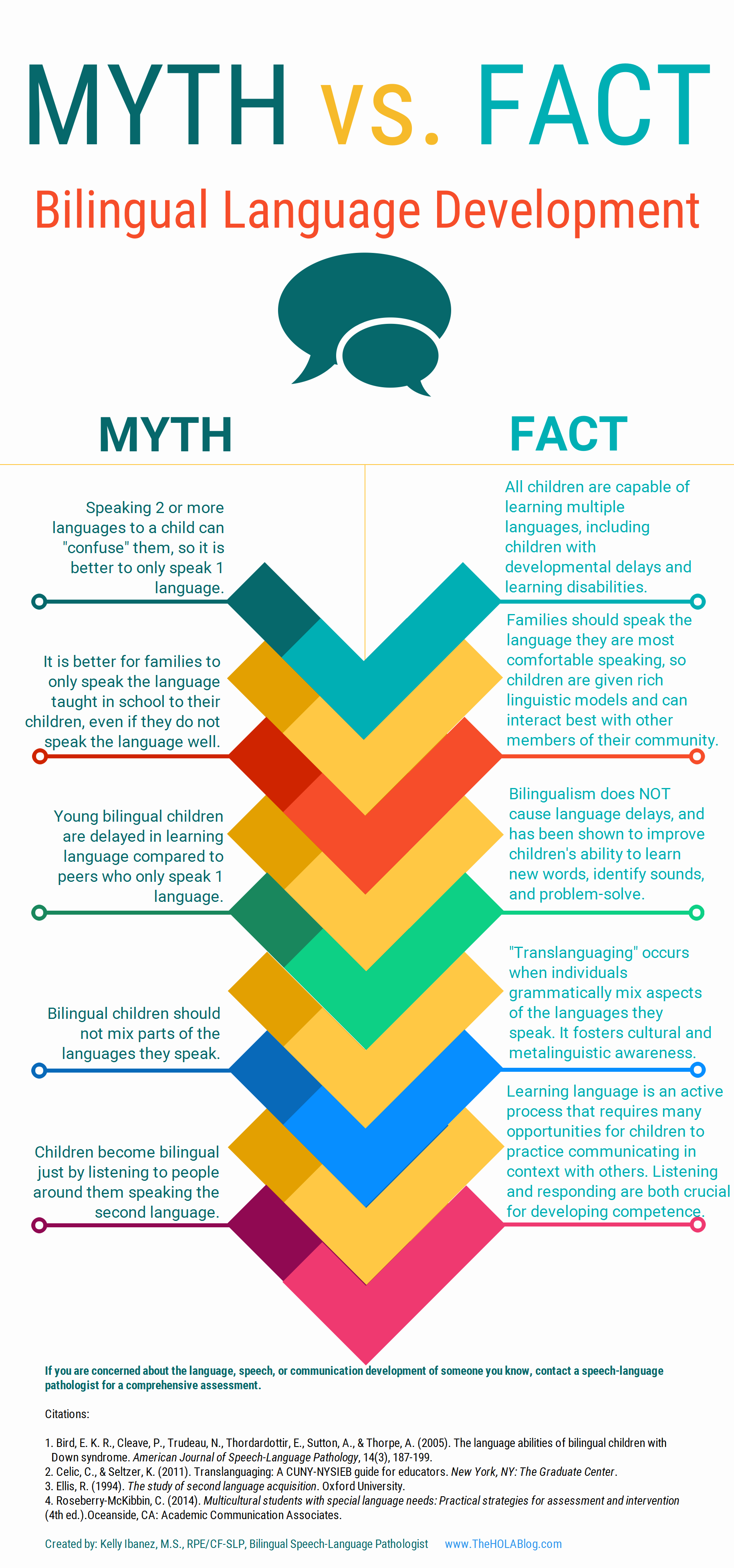 Let’s start with an excellent free infographic entitled from the Hola Blog “Myth vs. Fact: Bilingual Language Development” which was created by Kelly Ibanez, MS CCC-SLP to help dispel bilingual myths and encourage practices that promote multilingualism. Clinicians can download it and refer to it themselves, share it with other health and/or educational professionals as well as show it to parents of their clients.
Let’s start with an excellent free infographic entitled from the Hola Blog “Myth vs. Fact: Bilingual Language Development” which was created by Kelly Ibanez, MS CCC-SLP to help dispel bilingual myths and encourage practices that promote multilingualism. Clinicians can download it and refer to it themselves, share it with other health and/or educational professionals as well as show it to parents of their clients.
Let us now move on to the typical phonological development of English speaking children. After all, in order to compare other languages to English, SLPs need to be well versed in the acquisition of speech sounds in the English language. Children’s speech acquisition, developed by Sharynne McLeod, Ph.D., of Charles Sturt University, is one such resource. It contains a compilation of data on typical speech development for English speaking children, which is organized according to children’s ages to reflect a typical developmental sequence.
 Next up, is a great archive which contains phonetic inventories of the various language spoken around the world for contrastive analysis purposes. The same website also contains a speech accent archive. Native and non-native speakers of English were recorded reading the same English paragraph for teaching and research purposes. It is meant to be used by professionals who are interested in comparing the accents of different English speakers.
Next up, is a great archive which contains phonetic inventories of the various language spoken around the world for contrastive analysis purposes. The same website also contains a speech accent archive. Native and non-native speakers of English were recorded reading the same English paragraph for teaching and research purposes. It is meant to be used by professionals who are interested in comparing the accents of different English speakers.
![]() Now let’s talk about one of my favorite websites, MULTILINGUAL CHILDREN’S SPEECH, also developed by Dr. Mcleod of Charles Stuart University. It contains an AMAZING plethora of resources on bilingual speech development and assessment. To illustrate, its Speech Acquisition Data includes A list of over 200 speech acquisition studies. It also contains a HUGE archive on Speech Assessments in NUMEROUS LANGUAGES as well as select assessment reviews. Finally, the website also lists in detail how aspects of speech (e.g., consonants, vowels, syllables, tones) differ between languages.
Now let’s talk about one of my favorite websites, MULTILINGUAL CHILDREN’S SPEECH, also developed by Dr. Mcleod of Charles Stuart University. It contains an AMAZING plethora of resources on bilingual speech development and assessment. To illustrate, its Speech Acquisition Data includes A list of over 200 speech acquisition studies. It also contains a HUGE archive on Speech Assessments in NUMEROUS LANGUAGES as well as select assessment reviews. Finally, the website also lists in detail how aspects of speech (e.g., consonants, vowels, syllables, tones) differ between languages.
The Leader’s Project Website is another highly informative source of FREE information on bilingual assessments, intervention, and FREE CEUS.
Now, I’d like to list some resources regarding language transfer errors.
This chart from Cengage Learning contains a nice, concise Language Guide to Transfer Errors. While it is aimed at multilingual/ESL writers, the information contained on the site is highly applicable to multilingual speakers as well.
You can also find a bonus transfer chart HERE. It contains information on specific structures such as articles, nouns, verbs, pronouns, adverbs, adjectives, word order, questions, commands, and negatives on pages 1-6 and phonemes on pages 7-8.
A final bonus chart entitled: Teacher’s Resource Guide of Language Transfer Issues for English Language Learners containing information on grammar and phonics for 10 different languages can be found HERE.
Similarly, this 16-page handout: Language Transfers: The Interaction Between English and Students’ Primary Languages also contains information on phonics and grammar transfers for Spanish, Cantonese, Vietnamese, Hmong Korean, and Khmer languages.
 For SLPs working with Russian-speaking children the following links pertinent to assessment, intervention and language transference may be helpful:
For SLPs working with Russian-speaking children the following links pertinent to assessment, intervention and language transference may be helpful:
- Working with Russian-speaking clients: implications for speech-language assessment
- Strategies in the acquisition of segments and syllables in Russian-speaking children
- Language Development of Bilingual Russian/ English Speaking Children Living in the United States: A Review of the Literature
- The acquisition of syllable structure by Russian-speaking children with SLI
To determine information about the children’s language development and language environment, in both their first and second language, visit the CHESL Centre website for The Alberta Language Development Questionnaire and The Alberta Language Environment Questionnaire
There you have it! FREE bilingual/multicultural SLP resources compiled for you conveniently in one place. And since there are much more FREE GEMS online, I’d love it if you guys contributed to and expanded this modest list by posting links and title descriptions in the comments section below for others to benefit from!
Together we can deliver the most up to date evidence-based assessment and intervention to bilingual and multicultural students that we serve! Click HERE to check out the FREE Resources in the SLPs for Evidence-Based Practice Group
Helpful Bilingual Smart Speech Therapy Resources:
- Checklist for Identification of Speech-Language Disorders in Bilingual and Multicultural Children
- Multicultural Assessment Bundle
- Best Practices in Bilingual Literacy Assessments and Interventions
- Dynamic Assessment of Bilingual and Multicultural Learners in Speech-Language Pathology
- Practical Strategies for Monolingual SLPs Assessing and Treating Bilingual Children
- Language Difference vs. Language Disorder: Assessment & Intervention Strategies for SLPs Working with Bilingual Children
- Impact of Cultural and Linguistic Variables On Speech-Language Services
- Assessment of sound and syllable imitation in Russian-speaking infants and toddlers
- Russian Articulation Screener
- Creating Translanguaging Classrooms and Therapy Rooms
Why Are My Child’s Test Scores Dropping?
 “I just don’t understand,” says a parent bewilderingly, “she’s receiving so many different therapies and tutoring every week, but her scores on educational, speech-language, and psychological testing just keep dropping!”
“I just don’t understand,” says a parent bewilderingly, “she’s receiving so many different therapies and tutoring every week, but her scores on educational, speech-language, and psychological testing just keep dropping!”
I hear a variation of this comment far too frequently in both my private practice as well as outpatient school in hospital setting, from parents looking for an explanation regarding the decline of their children’s standardized test scores in both cognitive (IQ) and linguistic domains. That is why today I wanted to take a moment to write this blog post to explain a few reasons behind this phenomenon.
Children with language impairments represent a highly diverse group, which exists along a continuum. Some children’s deficits may be mild while others far more severe. Some children may receive very little intervention services and thrive academically, while others can receive inordinate amount of interventions and still very limitedly benefit from them. To put it in very simplistic terms, the above is due to two significant influences – the interaction between the child’s (1) genetic makeup and (2) environmental factors.
There is a reason why language disorders are considered developmental. Firstly, these difficulties are apparent from a young age when the child’s language just begins to develop. Secondly, the trajectory of the child’s language deficits also develops along with the child and can progress/lag based on the child’s genetic predisposition, resiliency, parental input, as well as schooling and academically based interventions.
Let us discuss some of the reasons why standardized testing results may decline for select students who are receiving a variety of support services and interventions.
Ineffective Interventions due to Misdiagnosis
Sometimes, lack of appropriate/relevant intervention provision may be responsible for it. Let’s take an example of a misdiagnosis of alcohol related deficits as Autism, which I have frequently encountered in my private practice, when performing second opinion testing and consultations. Unfortunately, the above is not uncommon. Many children with alcohol-related impairments may present with significant social emotional dysregulation coupled with significant externalizing behavior manifestations. As a result, without a thorough differential diagnosis they may be frequently diagnosed with ASD and then provided with ABA therapy services for years with little to no benefit.
Ineffective Interventions due to Lack of Comprehensive Testing
Let us examine another example of a student with average intelligence but poor reading performance. The student may do well in school up to certain grade but then may begin to flounder academically. Because only the student’s reading abilities ‘seem’ to be adversely impacted, no comprehensive language and literacy evaluations are performed. The student may receive undifferentiated extra reading support in school while his scores may continue to drop.
Once the situation ‘gets bad enough’, the student’s language and literacy abilities may be comprehensively assessed. In a vast majority of situations these type of assessments yield the following results:
- The student’s oral language expression as well as higher order language abilities are adversely affected and require targeted language intervention
- The undifferentiated reading intervention provided to the student was NOT targeting actual areas of weaknesses
As can be seen from above examples, targeted intervention is hugely important and, in a number of cases, may be responsible for the student’s declining performance. However, that is not always the case.
What if it was definitively confirmed that the student was indeed diagnosed appropriately and was receiving quality services but still continued to decline academically. What then?
Well, we know that many children with genetic disorders (Down Syndrome, Fragile X, etc.) as well as intellectual disabilities (ID) can make incredibly impressive gains in a variety of developmental areas (e.g., gross/fine motor skills, speech/language, socio-emotional, ADL, etc.) but their gains will not be on par with peers without these diagnoses.
The situation becomes much more complicated when children without ID (or with mild intellectual deficits) and varying degrees of language impairment, receive effective therapies, work very hard in therapy, yet continue to be perpetually behind their peers when it comes to making academic gains. This occurs because of a phenomenon known as Cumulative Cognitive Deficit (CCD).
The Effect of Cumulative Cognitive Deficit (CCD) on Academic Performance
According to Gindis (2005) CCD “refers to a downward trend in the measured intelligence and/or scholastic achievement of culturally/socially disadvantaged children relative to age-appropriate societal norms and expectations” (p. 304). Gindis further elucidates by quoting Satler (1992): “The theory behind cumulative deficit is that children who are deprived of enriching cognitive experiences during their early years are less able to profit from environmental situations because of a mismatch between their cognitive schemata and the requirements of the new (or advanced) learning situation” (pp. 575-576).
So who are the children potentially at risk for CCD?
One such group are internationally (and domestically) adopted as well as foster care children. A number of studies show that due to the early life hardships associated with prenatal trauma (e.g., maternal substance abuse, lack of adequate prenatal care, etc.) as well as postnatal stress (e.g., adverse effect of institutionalization), many of these children have much poorer social and academic outcomes despite being adopted by well-to-do, educated parents who continue to provide them with exceptional care in all aspects of their academic and social development.
Another group, are children with diagnosed/suspected psychiatric impairments and concomitant overt/hidden language deficits. Depending on the degree and persistence of the psychiatric impairment, in addition to having intermittent access to classroom academics and therapy interventions, the quality of their therapy may be affected by the course of their illness. Combined with sporadic nature of interventions this may result in them falling further and further behind their peers with respect to social and academic outcomes.
A third group (as mentioned previously) are children with genetic syndromes, neurodevelopmental disorders (e.g., Autism) and intellectual disabilities. Here, it is very important to explicitly state that children with diagnosed or suspected alcohol related deficits (FASD) are particularly at risk due to the lack of consensus/training regarding FAS detection/diagnosis. Consequently, these children may evidence a steady ‘decline’ on standardized testing despite exhibiting steady functional gains in therapy.
Brief Standardized Testing Score Tutorial:
When we look at norm-referenced testing results, score interpretation can be quite daunting. For the sake of simplicity, I’d like to restrict this discussion to two types of scores: raw scores and standard scores.
The raw score is the number of items the child answered correctly on a test or a subtest. However, raw scores need to be interpreted to be meaningful. For example, a 9 year old student can attain a raw score of 12 on a subtest of a particular test (e.g., Listening Comprehension Test-2 or LCT-2). Without more information, the raw score has no meaning. If the test consisted of 15 questions, a raw score of 12 would be an average score. Alternatively, if the subtest had 36 questions, a raw score of 12 would be significantly below-average (e.g., Test of Problem Solving-3 or TOPS-3).
Consequently, the raw score needs to be converted to a standard score. Standard scores compare the student’s performance on a test to the performance of other students his/her age. Many standardized language assessments have a mean of 100 and a standard deviation of 15. Thus, scores between 85 and 115 are considered to be in the average range of functioning.
Now lets discuss testing performance variation across time. Let’s say an 8.6 year old student took the above mentioned LCT-2 and attained poor standard scores on all subtests. That student qualifies for services and receives them for a period of one year. At that time the LCT-2 is re-administered once again and much to the parents surprise the student’s standard scores appear to be even lower than when he had taken the test as an eight year old (illustration below).
Results of The Listening Comprehension Test -2 (LCT-2): Age: 8:4
| Subtests | Raw Score | Standard Score | Percentile Rank | Description |
| Main Idea | 5 | 67 | 2 | Severely Impaired |
| Details | 2 | 63 | 1 | Severely Impaired |
| Reasoning | 2 | 69 | 2 | Severely Impaired |
| Vocabulary | 0 | Below Norms | Below Norms | Profoundly Impaired |
| Understanding Messages | 0 | <61 | <1 | Profoundly Impaired |
| Total Test Score | 9 | <63 | 1 | Profoundly Impaired |
(Mean = 100, Standard Deviation = +/-15)
Results of The Listening Comprehension Test -2 (LCT-2): Age: 9.6
| Subtests | Raw Score | Standard Score | Percentile Rank | Description |
| Main Idea | 6 | 60 | 0 | Severely Impaired |
| Details | 5 | 66 | 1 | Severely Impaired |
| Reasoning | 3 | 62 | 1 | Severely Impaired |
| Vocabulary | 4 | 74 | 4 | Moderately Impaired |
| Understanding Messages | 2 | 54 | 0 | Profoundly Impaired |
| Total Test Score | 20 | <64 | 1 | Profoundly Impaired |
(Mean = 100, Standard Deviation = +/-15)
However, if one looks at the raw score column on the far left, one can see that the student as a 9 year old actually answered more questions than as an 8 year old and his total raw test score went up by 11 points.
The above is a perfect illustration of CCD in action. The student was able to answer more questions on the test but because academic, linguistic, and cognitive demands continue to steadily increase with age, this quantitative improvement in performance (increase in total number of questions answered) did not result in qualitative improvement in performance (increase in standard scores).
In the first part of this series I have introduced the concept of Cumulative Cognitive Deficit and its effect on academic performance. Stay tuned for part II of this series which describes what parents and professionals can do to improve functional performance of students with Cumulative Cognitive Deficit.
References:
- Bowers, L., Huisingh, R., & LoGiudice, C. (2006). The Listening Comprehension Test-2 (LCT-2). East Moline, IL: LinguiSystems, Inc.
- Bowers, L., Huisingh, R., & LoGiudice, C. (2005). The Test of Problem Solving 3-Elementary (TOPS-3). East Moline, IL: LinguiSystems.
- Gindis, B. (2005). Cognitive, language, and educational issues of children adopted from overseas orphanages. Journal of Cognitive Education and Psychology, 4 (3): 290-315.
- Sattler, J. M. (1992). Assessment of Children. Revised and updated 3rd edition. San Diego: Jerome M. Sattler.
