 Having a solid vocabulary knowledge is key to academic success. Vocabulary is the building block of language. It allows us to create complex sentences, tell elaborate stories as well as write great essays. Having limited vocabulary is primary indicator of language learning disability, which in turn blocks students from obtaining critical literacy skills necessary for reading, writing, and spelling. “Indeed, one of the , most enduring findings in reading research is the extent to which students’ vocabulary knowledge relates to their reading comprehension” (Osborn & Hiebert, 2004)
Having a solid vocabulary knowledge is key to academic success. Vocabulary is the building block of language. It allows us to create complex sentences, tell elaborate stories as well as write great essays. Having limited vocabulary is primary indicator of language learning disability, which in turn blocks students from obtaining critical literacy skills necessary for reading, writing, and spelling. “Indeed, one of the , most enduring findings in reading research is the extent to which students’ vocabulary knowledge relates to their reading comprehension” (Osborn & Hiebert, 2004)
Teachers and SLPs frequently inquire regarding effective vocabulary instruction methods for children with learning disabilities. However, what some researchers have found when they set out to “examine how oral vocabulary instruction was enacted in kindergarten” was truly alarming.
In September 2014, Wright and Neuman, analyzed about 660 hours of observations over a course of 4 days (12 hours) in 55 classrooms in a range of socio-economic status schools.
They found that teachers explained word meanings during “teachable moments” in the context of other instruction.
They also found that teachers:
- Gave one-time, brief word explanations
- Engaged in unsystematic word selection
- And spent minimal time on vocabulary devoted to subject areas (e.g., science and social studies in which word explanations were most dense)
They also found an economic status discrepancy, namely:
Teachers serving in economically advantaged schools explained words more often and were more likely to address sophisticated words than teachers serving in economically disadvantaged schools.
They concluded that “these results suggest that the current state of instruction may be CONTRIBUTING to rather than ameliorating vocabulary gaps by socioeconomic status.”
Similar findings were reported by other scholars in the field who noted that “teachers with many struggling children often significantly reduce the quality of their own vocabulary unconsciously to ensure understanding.” So they “reduce the complexity of their vocabulary drastically.” “For many children the teacher is the highest vocabulary example in their life. It’s sort of like having a buffet table but removing everything except a bowl of peanuts-that’s all you get“. (Excerpts from Anita Archer’s Interview with Advance for SLPs)
It is important to note that vocabulary gains are affected by socioeconomic status as well as maternal education level. Thus, children whose family incomes are at or below the poverty level fare much more poorly in the area of vocabulary acquisition than middle class children. Furthermore, Becker (2011) found that children of higher educated parents can improve their vocabulary more strongly than children whose parents have a lower educational level.
Limitations of Poor Readers:
Poor readers often lack adequate vocabulary to get meaning from what they read. To them, reading is difficult and tedious, and they are unable (and often unwilling) to do the large amount of reading they must do if they are to encounter unknown words often enough to learn them.
Matthew Effect, “rich get richer, poor get poorer”, or interactions with the environment exaggerate individual differences over time. Good readers read more, become even better readers, and learn more words. Poor readers read less, become poorer readers, and learn fewer words. The vocabulary problems of students who enter school with poorer limited vocabularies only exacerbate over time.
However, even further exacerbating the issue is that students from low SES households have limited access to books. 61% of low-income families have NO BOOKS at all in their homes for their children (Reading Literacy in the United States: Findings from the IEA Reading Literacy Study, 1996.) In some under-resourced communities, there is ONLY 1 book for every 300 children. Neuman, S., & Dickinson, D. (Eds.). (2006) Handbook of Early Literacy Research (Vol. 2). In contrast, the average middle class child has 13+ books in the home.
The above discrepancy can be effectively addressed by holding book drives to raise books for under privileged students and their siblings. Instructions for successful book drives HERE.
So what are effective methods of vocabulary instruction for children with language impairments?
According to (NRP, 2000) a good way for students to learn vocabulary directly is to explicitly teach them individual words and word-learning strategies .
For children with low initial vocabularies, approaches that teach word meanings as part of a semantic field are found to be especially effective (Marmolejo, 1991).
Many vocabulary scholars (Archer, 2011; Biemiller, 2004; Gunning 2004, etc.) agree on a number of select instructional strategies which include:
- Rich experiences/high classroom language related to the student experience/interests
- Explicit vs. incidental instruction with frequent exposure to words
- Instructional routine for vocabulary
- Establishing word relationships
- Word-learning strategies to impart depth of meaning
- Morphological awareness instruction
Response to Intervention: Improving Vocabulary Outcomes
.JPG)
For students with low vocabularies, to attain the same level of academic achievement as their peers on academic coursework of language arts, reading, and written composition, targeted Tier II intervention may be needed.
Tier II words are those for which children have an understanding of the underlying concepts, are useful across a variety of settings and can be used instructionally in a variety of ways
According to Beck et al 2002, Tier II words should be the primary focus of vocabulary instruction, as they would make the most significant impact on a child’s spoken and written expressive capabilities.
Tier II vocabulary words
- High frequency words which occur across a variety of domains conversations, text, etc.
- Contain multiple meanings
- Descriptive in nature
- Most important words for direct instruction as they facilitate academic success
- Hostile, illegible, tolerate, immigrate, tremble, despicable, elapse, etc.
According to Judy Montgomery “You can never select the wrong words to teach.”
Vocabulary Selection Tips:
- Make it thematic
- Embed it in current events (e.g., holidays, elections, seasonal activities, etc)
- Classroom topic related (e.g., French Revolution, the Water Cycle, Penguin Survival in the Polar Regions, etc)
- Do not select more than 4-5 words to teach per unit to not overload the working memory (Robb, 2003)
- Select difficult/unknown words that are critical to the passage meaning, which the students are likely to use in the future (Archer, 2015)
- Select words used across many domains
Examples of Spring Related Vocabulary
Adjectives:
- Flourishing
- Lush
- Verdant
- Refreshing
Nouns:
- Allergies
- Regeneration
- Outdoors
- Seedling
- Sapling
Verbs
- Awaken
- Teem
- Romp
- Rejuvenate
Idiomatic Expressions:
- April Showers Bring May Flowers
- Green Thumb
- Spring Chicken
- Spring Into Action
Creating an Effective Vocabulary Intervention Packets and Materials
Sample Activity Suggestions:
- Text Page (story introducing the topic containing context embedded words)

- Vocabulary Page (list of story embedded words their definitions, and what parts of speech the words are)
- Multiple Choice Questions or Open Ended Questions Page
- Crossword Puzzle Page
- Fill in the Blank Page
- True (one word meaning) Synonym/Antonym Matching Page
- Explain the Multiple Meaning of Words Page
- Create Complex Sentences Using Story Vocabulary Page
Intervention Technique Suggestions:
1.Read vocabulary words in context embedded in relevant short texts
2.Teach individual vocabulary words directly to comprehend classroom-specific texts (definitions)
3.Provide multiple exposures of vocabulary words in multiple contexts, (synonyms, antonyms, multiple meaning words, etc.)
4.Maximize multisensory intervention when learning vocabulary to maximize gains (visual, auditory, tactile, etc.)
5.Use multiple instructional methods for a range of vocabulary learning tasks and outcomes (read it, spell it, write it in a sentence, practice with a friend, etc.)
6.Use morphological awareness instruction (post to follow)
- An ability to recognize, understand, and use word parts (prefixes, suffixes that “carry significance” when speaking and in reading tasks
Conclusion:
Having the right tools for the job is just a small first step in the right direction of creating a vocabulary-rich environment even for the most disadvantaged learners. So Happy Speeching!

Helpful Smart Speech Resources:
 Today I’m excited to introduce a new product: “Creating A Learning Rich Environment for Language Delayed Preschoolers“. This 40 page presentation provides suggestions to parents regarding how to facilitate further language development in language delayed/impaired preschoolers at home in conjunction with existing outpatient, school, or private practice based speech language services. It details implementation strategies as well as lists useful materials, books, and websites of interest.
Today I’m excited to introduce a new product: “Creating A Learning Rich Environment for Language Delayed Preschoolers“. This 40 page presentation provides suggestions to parents regarding how to facilitate further language development in language delayed/impaired preschoolers at home in conjunction with existing outpatient, school, or private practice based speech language services. It details implementation strategies as well as lists useful materials, books, and websites of interest. Last year an esteemed colleague, Dr. Roseberry-McKibbin posed this question in our
Last year an esteemed colleague, Dr. Roseberry-McKibbin posed this question in our 




 Recently, I’ve published an article in
Recently, I’ve published an article in  A few days ago I was asked by my higher-ups for a second opinion on a consult regarding a psychological evaluation on an 11-year-old boy, which was depicting a certain pattern of deficits without a reasonable justification as to why they were occurring. I had a working hypothesis but needed more evidence to turn it into a viable theory. So I set out to collect more evidence by interviewing a few ancillary professionals who were providing therapy services to the student.
A few days ago I was asked by my higher-ups for a second opinion on a consult regarding a psychological evaluation on an 11-year-old boy, which was depicting a certain pattern of deficits without a reasonable justification as to why they were occurring. I had a working hypothesis but needed more evidence to turn it into a viable theory. So I set out to collect more evidence by interviewing a few ancillary professionals who were providing therapy services to the student.


 In my social pragmatic language groups I target a wide variety of social communication goals for children with varying levels and degrees of impairment with a focus on improving their social pragmatic language competence. In the past I have written blog posts on a variety of social pragmatic language therapy topics, including strategies for
In my social pragmatic language groups I target a wide variety of social communication goals for children with varying levels and degrees of impairment with a focus on improving their social pragmatic language competence. In the past I have written blog posts on a variety of social pragmatic language therapy topics, including strategies for 


.JPG)







 The Test of Silent Word Reading Fluency (TOSWRF-2)
The Test of Silent Word Reading Fluency (TOSWRF-2)  With the passing of
With the passing of 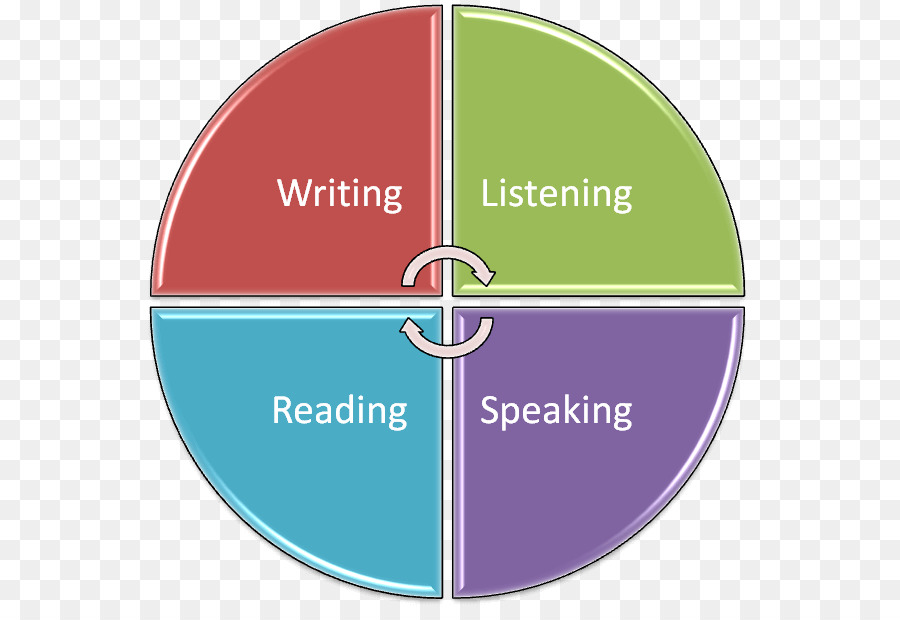 LANGUAGE TESTING
LANGUAGE TESTING Frequently, I see a variation of the following scenario on many speech and language forums.
Frequently, I see a variation of the following scenario on many speech and language forums. Let’s begin by answering a few simple questions. Was a thorough language evaluation with an emphasis on the child’s social pragmatic language abilities been completed? And by thorough, I am not referring to general language tests but to a variety of formal and informal social pragmatic language testing (read more
Let’s begin by answering a few simple questions. Was a thorough language evaluation with an emphasis on the child’s social pragmatic language abilities been completed? And by thorough, I am not referring to general language tests but to a variety of formal and informal social pragmatic language testing (read more  Please note that none of the general language tests such as the Preschool Language Scale-5 (PLS-5), Comprehensive Assessment of Spoken Language (CASL-2), the Test of Language Development-4 (TOLD-4) or even the Clinical Evaluation of Language Fundamentals Tests (CELF-P2)/ (CELF-5) tap into the child’s social language competence because they do NOT directly test the child’s social language skills (e.g., CELF-5 assesses them via a parental/teachers questionnaire). Thus, many children can attain average scores on these tests yet still present with pervasive social language deficits. That is why it’s very important to thoroughly assess social pragmatic language abilities of all children (no matter what their age is) presenting with behavioral deficits.
Please note that none of the general language tests such as the Preschool Language Scale-5 (PLS-5), Comprehensive Assessment of Spoken Language (CASL-2), the Test of Language Development-4 (TOLD-4) or even the Clinical Evaluation of Language Fundamentals Tests (CELF-P2)/ (CELF-5) tap into the child’s social language competence because they do NOT directly test the child’s social language skills (e.g., CELF-5 assesses them via a parental/teachers questionnaire). Thus, many children can attain average scores on these tests yet still present with pervasive social language deficits. That is why it’s very important to thoroughly assess social pragmatic language abilities of all children (no matter what their age is) presenting with behavioral deficits.
