
What are social pragmatic language deficits and how do they impact international adoptees years post adoption?
Scenario: John is a bright 11 year old boy who was adopted at the age of 3 from Russia by American parents. John’s favorite subject is math, he is good at sports but his most dreaded class is language arts. John has trouble understanding abstract information or summarizing what he has seen, heard or read. John’s grades are steadily slipping and his reading comprehension is below grade level. He has trouble retelling stories and his answers often raise more questions due to being very confusing and difficult to follow. John has trouble maintaining friendships with kids his age, who consider him too immature and feel like he frequently “misses the point” due to his inability to appropriately join play activities and discussions, understand non-verbal body language, maintain conversations on age-level topics, or engage in perspective taking (understand other people’s ideas, feelings, and thoughts). John had not received speech language services immediately post adoption despite exhibiting a severe speech and language delay at the time of adoption. The parents were told that “he’ll catch up quickly”, and he did, or so it seemed, at the time. John is undeniably bright yet with each day he struggles just a little bit more with understanding those around him and getting his point across. John’s scores were within normal limits on typical speech and language tests administered at his school, so he did not qualify for school based speech language therapy. Yet John clearly needs help.
John’s case is by no means unique. Numerous adopted children begin to experience similar difficulties; years post adoption, despite seemingly appropriate early social and academic development. What has many parents bewildered is that often times these difficulties are not glaringly pronounced in the early grades, which leads to delayed referral and lack of appropriate intervention for prolonged period of time.
The name for John’s difficulty is pragmatic language impairment, a diagnosis that has been the subject of numerous research debates since it was originally proposed in 1983 by Rapin and Allen.
So what is pragmatic language impairment and how exactly does it impact the child’s social and academic language abilities?
In 1983, Rapin and Allen proposed a classification of children with developmental language disorders. As part of this classification they described a syndrome of language impairment which they termed ‘semantic–pragmatic deficit syndrome’. Children with this disorder were described as being overly verbose, having poor turn–taking skills, poor discourse and narrative skills as well as having difficulty with topic initiation, maintenance and termination. Over the years the diagnostic label for this disorder has changed several times, until it received its current name “pragmatic language impairment” (Bishop, 2000).
Pragmatic language ability involves the ability to appropriately use language (e.g., persuade, request, inform, reject), change language (e.g., talk differently to different audiences, provide background information to unfamiliar listeners, speak differently in different settings, etc) as well as follow conversational rules (e.g., take turns, introduce topics, rephrase sentences, maintain appropriate physical distance during conversational exchanges, use facial expressions and eye contact, etc) all of which culminate into the child’s general ability to appropriately interact with others in a variety of settings.
For most typically developing children, the above comes naturally. However, for children with pragmatic language impairment appropriate social interactions are not easy. Children with pragmatic language impairment often misinterpret social cues, make inappropriate or off-topic comments during conversations, tell stories in a disorganized way, have trouble socially interacting with peers, have difficulty making and keeping friends, have difficulty understanding why they are being rejected by peers, and are at increased risk for bullying.
So why do adopted children experience social pragmatic language deficits many years post adoption?
Well for one, many internationally adopted children are at high risk for developmental delay because of their exposure to institutional environments. Children in institutional care often experience neglect, lack of language stimulation, lack of appropriate play experiences, lack of enriched community activities, as well as inadequate learning settings all of which has long lasting negative impact on their language development including the development of their pragmatic language skills (especially if they are over 3 years of age). Furthermore, other, often unknown, predisposing factors such as medical, genetic, and family history can also play a negative role in pragmatic language development, since at the time of adoption very little information is known about the child’s birth parents or maternal prenatal care.
Difficulty with detection as well as mistaken diagnoses of pragmatic language impairment
Whereas detecting difficulties with language content and form is relatively straightforward, pragmatic language deficits are more difficult to detect, because pragmatics are dependent on specific contexts and implicit rules. While many children with pragmatic language impairment will present with poor reading comprehension, low vocabulary, and grammar errors (pronoun reversal, tense confusion) in addition to the already described deficits, not all the children with pragmatic language impairment will manifest the above signs. Moreover, while pragmatic language impairment is diagnosed as one of the primary difficulties in children on autistic spectrum, it can manifest on its own without the diagnosis of autism. Furthermore, due to its complicated constellation of symptoms as well as frequent coexistence with other disorders, pragmatic language impairment as a standalone diagnosis is often difficult to establish without the multidisciplinary team involvement (e.g., to rule out associated psychiatric and neurological impairment).
It is also not uncommon for pragmatic language deficits to manifest in children as challenging behaviors (and in severe cases be misdiagnosed due to the fact that internationally adopted children are at increased risk for psychiatric disorders in childhood, adolescence and adulthood). Parents and teachers often complain that these children tend to “ignore” presented directions, follow their own agenda, and frequently “act out inappropriately”. Unfortunately, since children with pragmatic language impairment rely on literal communication, they tend to understand and carry out concrete instructions and tasks versus understanding indirect requests which contain abstract information. Additionally, since perspective taking abilities are undeveloped in these children, they often fail to understand and as a result ignore or disregard other people’s feelings, ideas, and thoughts, which may further contribute to parents’ and teachers’ beliefs that they are deliberately misbehaving.
Due to difficulties with detection, pragmatic language deficits can persist undetected for several years until they are appropriately diagnosed. What may further complicate detection is that a certain number of children with pragmatic language deficits will perform within the normal range on typical speech and language testing. As a result, unless a specific battery of speech language tests is administered that explicitly targets the identification of pragmatic language deficits, some of these children may be denied speech and language services on the grounds that their total language testing score was too high to qualify them for intervention.
How to initiate an appropriate referral process if you suspect that your school age child has pragmatic language deficits?
When a child is presenting with a number of above described symptoms, it is recommended that a medical professional such as a neurologist or a psychologist be consulted in order to rule out other more serious diagnoses. Then, the speech language pathologist can perform testing in order to confirm the presence of pragmatic language impairment as well as determine whether any other linguistically based deficits coexist with it. Furthermore, even in cases when the pragmatic language impairment is a secondary diagnosis (e.g. Autism) the speech language pathologist will still need to be involved in order to appropriately address the social linguistic component of this deficit.
To obtain appropriate speech and language testing in a school setting, the first step that parents can take is to consult with the classroom teacher. For the school age child (including preschool and kindergarten) the classroom teacher can be the best parental ally. After all both parents and teachers know the children quite well and can therefore take into account their behavior and functioning in a variety of social and academic contexts. Once the list of difficulties and inappropriate behaviors has been compiled, and both parties agree that the “red flags” merit further attention, the next step is to involve the school speech language pathologist (make a referral) to confirm the presence and/or severity of the impairment via speech language testing.
When attempting to confirm/rule out pragmatic language impairment, the speech language pathologist has the option of using a combination of formal and informal assessments including parental questionnaires, discourse and narrative analyses as well as observation checklists.
Below is the list of select formal and informal speech language assessment instruments which are sensitive to detection of pragmatic language impairment in children as young as 4-5 years of age.
1. Children’s Communication Checklist-2 (CCC–2) (Available: Pearson Publication)
2. Test of Narrative Development (TNL) (Available: Linguisystems Publication)
3. Test of Language Competence Expanded Edition (TLC-E) (Available: Pearson Publication)
4. Test of Pragmatic Language-2 (TOPL-2) (Available: Linguisystems Publication)
5. Social Emotional Evaluation (SEE) (Available: Super Duper Publication)
6. Dynamic Informal Social Thinking Assessment (www.socialthinking.com)
7. Social Language Development Test -Elementary (SLDT-E) (Available: Linguisystems Publication)
8. Social Language Development Test -Adolescent (SLDT-A) (Available: Linguisystems Publication)
It is also very important to note that several formal and informal instruments and analyses need to be administered/performed in order to create a complete diagnostic picture of the child’s deficits.
When to seek private pragmatic language evaluation and therapy services?
Unfortunately, the process of obtaining appropriate social pragmatic assessment in a school setting is often fraught with numerous difficulties. For one, due to financial constraints, not all school districts possess the appropriate, up to date pragmatic language testing instruments.
Another issue is the lack of time. To administer comprehensive assessment which involves 2-3 different assessment instruments, an adequate amount of time (e.g., 2+ hours) is needed in order to create the most comprehensive pragmatic profile for the child. School based speech language pathologists often lack this valuable commodity due to increased case load size (often seeing between 45 to 60 students per week), which leaves them with very limited time for testing.
Further complicating the issue are the special education qualification rules, which are different not just from state to state but in some cases from one school district to the next within the same state. Some school districts strictly stipulate that the child’s performance on testing must be 1.5-2 standard deviations below the normal limits in order to qualify for therapy services.
But what if the therapist is not in possession of any formal assessment instruments and can only do informal assessment?
And what happens to the child who is “not impaired enough” (e.g., 1 SD vs. 1.5 SD)?
Consequently, in recent years more and more parents are opting for private pragmatic language assessments and therapy for their children.
Certainly, there are numerous advantages for going via the private route. For one, parents are directly involved and directly influence the quality of care their children receive.
One advantage to private therapy is that parents can request to be present during the evaluation and therapy sessions. As such, not only do the parents get to understand the extent of the child’s impairment but they also learn valuable techniques and strategies they can utilize in home setting to facilitate carryover and skill generalization (how to ask questions, provide choices, etc).
Another advantage is the provision of individual therapy services in contrast to school based services which are generally attended by groups as large as 4-5 children per session. Here, some might disagree and state that isn’t the point of pragmatic therapy is for the child to practice his/her social skills with other children?
Absolutely! However, before a skill can be generalized it needs to be taught! Most children with pragmatic language impairment initially require individual sessions, in some of which it may be necessary to use drill work to teach a specific skill. Once the necessary skills are taught, only then can children be placed into social groups where they can practice generalizing their skills. Moreover, many of these children greatly benefit from being in group or play settings with typical peers and/or sibling tutors who may facilitate the generalization of the desired skill more naturally, all of which can be arranged within private therapy settings.
Yet another advantage to obtaining private therapy services is that there are some private clinics which are almost exclusively devoted to teaching social pragmatic communication and which offer a variety of therapeutic services including individual therapy, group therapy and even summer camps that target the improvement of pragmatic language and social communication skills.
The flexibility offered by private therapy is also important if a parent is seeking a specific social skills curriculum for their child (e.g., “Socially Speaking”) or if they are interested in social skill training that is based on the methods of specific researchers/authors (e.g., Michelle Garcia Winner MACCC-SLP; Dr. Jed Baker PhD, etc), which may not be offered by their child’s school.
There are many routes open for parents to pursue when it comes to their child’s pragmatic language assessment and intervention. However, the first step in that process is parental education!
To learn more about pragmatic language impairment please visit the ASHA website at www.asha.org and type in your query in the search window located in the upper right corner of the website. To find a professional specializing in assessment and treatment of pragmatic language disorders in your area please visit http://asha.org/proserv/.
References
Adams, C. (2001). “Clinical diagnostic and intervention studies of children with semantic-pragmatic language disorder.” International Journal of Language and Communication Disorders 36(3): 289-305.
Bishop, D. V. (1989). “Autism, Asperger’s syndrome and semantic-pragmatic disorder: Where are the boundaries?” British Journal of Disorders of Communication 24(2): 107-121.
Bishop, D. V. M. and G. Baird (2001). “Parent and teacher report of pragmatic aspects of communication: Use of the Children’s Communication Checklist in a clinical setting.” Developmental Medicine and Child Neurology 43(12): 809-818.
Botting, N., & Conti-Ramsden, G. (1999). Pragmatic language impairment without autism: The children in question. Autism, 3, 371–396.[
Brackenbury, T., & Pye, C. (2005). Semantic deficits in children with language impairments: Issues for clinical assessment. Language, Speech, and Hearing Services in Schools, 36, 5–16.
Burgess, S., & Turkstra, L. S. (2006). Social skills intervention for adolescents with autism spectrum disorders: A review of the experimental evidence. EBP Briefs, 1(4), 1–21.
Camarata, S., M., and T. Gibson (1999). “Pragmatic Language Deficits in Attention-Deficit Hyperactivity Disorder (ADHD).” Mental Retardation and Developmental Disabilities 5: 207-214.
Ketelaars, M. P., Cuperus, J. M., Jansonius, K., & Verhoeven, L. (2009). Pragmatic language impairment and associated behavioural problems. International Journal of Language and Communication Disorders, 45, 204–214.
Ketelaars, M. P., Cuperus, J. M., Van Daal, J., Jansonius, K., & Verhoeven, L. (2009). Screening for pragmatic language impairment: The potential of the Children’s Communication Checklist. Research in Developmental Disabilities, 30, 952–960.
Miniscalco, C., Hagberg, B., Kadesjö, B., Westerlund, M., & Gillberg, C. (2007). Narrative skills, cognitive profiles and neuropsychiatric disorders in 7-8-year-old children with late developing language. International Journal of Language and Communication Disorders, 42, 665–681.
Rapin I, Allen D (1983). Developmental language disorders: Nosologic considerations. In U. Kirk (Ed.), Neuropsychology of language, reading, and spelling (pp. 155–184). : Academic Press.
 I have to admit, I don’t really like flashcards. I especially don’t like it when parents or SLPs use flashcards to drill vocabulary in toddlers and preschoolers, much less school aged children. I feel that it produces very limited learnability and generalization. I am personally a proponent of thematic language learning, since it allows me to take a handful of words/concepts and reinforce them in a number of different ways. The clients still get the benefit of information repetition, much like one would get during a typical flashcard drill. However, they are also getting much more. Thematic language learning allows the client to increase word comprehension, make connections to real life scenarios, develop abstract thinking skills, as well as to transfer and generalize knowledge (Morrow, Pressley, Smith, & Smith, 1997; Ramey, 1995).
I have to admit, I don’t really like flashcards. I especially don’t like it when parents or SLPs use flashcards to drill vocabulary in toddlers and preschoolers, much less school aged children. I feel that it produces very limited learnability and generalization. I am personally a proponent of thematic language learning, since it allows me to take a handful of words/concepts and reinforce them in a number of different ways. The clients still get the benefit of information repetition, much like one would get during a typical flashcard drill. However, they are also getting much more. Thematic language learning allows the client to increase word comprehension, make connections to real life scenarios, develop abstract thinking skills, as well as to transfer and generalize knowledge (Morrow, Pressley, Smith, & Smith, 1997; Ramey, 1995).

 How does the boy feel about the flower?
How does the boy feel about the flower?

 The girl is laughing because someone did something nice for her?
The girl is laughing because someone did something nice for her?



 A to Z Jr– a game of early categorizations is recommended for players 5 – 10 years of age, but can be used with older children depending on their knowledge base. The object of the game is to cover all letters on your letter board by calling out words in specific categories before the timer runs out. This game can be used to
A to Z Jr– a game of early categorizations is recommended for players 5 – 10 years of age, but can be used with older children depending on their knowledge base. The object of the game is to cover all letters on your letter board by calling out words in specific categories before the timer runs out. This game can be used to  Tribond Jr – is another great game which purpose is to determine how 3 seemingly random items are related to one another. Good for older children 7-12 years of age it’s also great for problem solving and reasoning as some of the answers are not so straight forward (e.g., what do the clock, orange and circle have in common? Psst…they are all round)
Tribond Jr – is another great game which purpose is to determine how 3 seemingly random items are related to one another. Good for older children 7-12 years of age it’s also great for problem solving and reasoning as some of the answers are not so straight forward (e.g., what do the clock, orange and circle have in common? Psst…they are all round)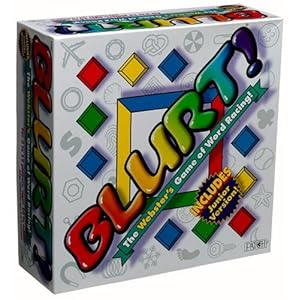 Blurt – a game for children 10 and up is a game that works on a simple premise. Blurt out as many answers as you can in order to guess what the word is. Blurt provides ready-made definitions that you read off to players so they could start guessing what the word is. Players and teams use squares on the board strategically to advance by competing in various definition challenges that increase language opportunities.
Blurt – a game for children 10 and up is a game that works on a simple premise. Blurt out as many answers as you can in order to guess what the word is. Blurt provides ready-made definitions that you read off to players so they could start guessing what the word is. Players and teams use squares on the board strategically to advance by competing in various definition challenges that increase language opportunities.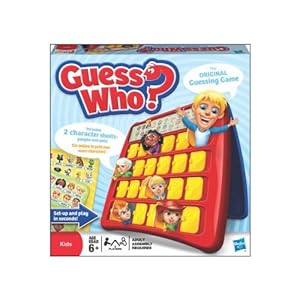 Guess Who (age 6+),
Guess Who (age 6+),  Guess Where (age 6+), and Mystery Garden (age 4+) are great for encouraging students to ask relevant questions in order to be the first to win the game. They are also terrific for encouraging reasoning skills. Questions have to be thought through carefully in order to be the first one to win the game.
Guess Where (age 6+), and Mystery Garden (age 4+) are great for encouraging students to ask relevant questions in order to be the first to win the game. They are also terrific for encouraging reasoning skills. Questions have to be thought through carefully in order to be the first one to win the game. 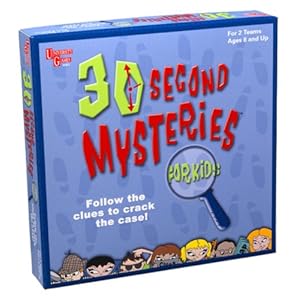 In 30 Second Mysteries kids need to use critical thinking and deductive reasoning in order to solve mysteriously sounding cases of everyday events. Each clue read aloud reveals more about the mystery and the trick is to solve it given the fewest number of clues in order to gain the most points.
In 30 Second Mysteries kids need to use critical thinking and deductive reasoning in order to solve mysteriously sounding cases of everyday events. Each clue read aloud reveals more about the mystery and the trick is to solve it given the fewest number of clues in order to gain the most points.







