
Recognizing the Warning Signs of Social Emotional Difficulties in Language Impaired Toddlers and Preschoolers



 September is practically here and many speech language pathologists (SLPs) are looking to efficiently prepare for assessing and treating a variety of clients on their caseloads.
September is practically here and many speech language pathologists (SLPs) are looking to efficiently prepare for assessing and treating a variety of clients on their caseloads.
With that in mind, a few years ago I created SLP Efficiency Bundles™, which are materials highly useful for SLPs working with pediatric clients. These materials are organized by areas of focus for efficient and effective screening, assessment, and treatment of speech and language disorders.
A. General Assessment and Treatment Start-Up Bundle contains 5 downloads for general speech language assessment and treatment planning and includes:
B. The Checklists Bundle contains 7 checklists relevant to screening and assessment in speech language pathology
C. Social Pragmatic Assessment and Treatment Bundle contains 6 downloads for social pragmatic assessment and treatment planning (from 18 months through school age) and includes:
D. Multicultural Assessment and Treatment Bundle contains 2 downloads relevant to assessment and treatment of bilingual/multicultural children
E. Narrative Assessment Bundle contains 3 downloads relevant to narrative assessment
F. Fetal Alcohol Spectrum Disorders Assessment and Treatment Bundle contains 3 downloads relevant to FASD assessment and treatment
G. Psychiatric Disorders Bundle contains 7 downloads relevant to language assessment and treatment in psychiatrically impaired children
You can find these bundles on SALE in my online store by clicking on the individual bundle links above. You can also purchase these products individually in my online store by clicking HERE.

 Back to school time is just around the corner and if your job is anything like mine then you are getting ready to perform a number of speech language screenings and assessments after the kids get back to school in September. In order to optimize the assessment process I’ve created a number of checklists and forms for my (and your convenience). They allow for quick and efficient determination of whether the preschool/school age monolingual/bilingual student in question requires any speech language services including: screening, assessment, future follow-up, or on-going monitoring. Please note that for bilingual students it is recommended that parents mark whether the child presents with deficits in one language or in both on the checklists (e.g., mark R, E, or B – Russian, English or both).
Back to school time is just around the corner and if your job is anything like mine then you are getting ready to perform a number of speech language screenings and assessments after the kids get back to school in September. In order to optimize the assessment process I’ve created a number of checklists and forms for my (and your convenience). They allow for quick and efficient determination of whether the preschool/school age monolingual/bilingual student in question requires any speech language services including: screening, assessment, future follow-up, or on-going monitoring. Please note that for bilingual students it is recommended that parents mark whether the child presents with deficits in one language or in both on the checklists (e.g., mark R, E, or B – Russian, English or both).
Speech Language Assessment Checklist For A Preschool Child is a 9 page guide created to assist speech language pathologists in the decision making process of how to select assessment instruments and prioritize assessment for preschool children 3:00-5:11 years of age. The goal is to eliminate administration of unnecessary or irrelevant tests and focus on the administration of instruments directly targeting the areas of difficulty that the child presents with.
It contains:
Checklist Target Areas:
Speech Language Assessment Checklist For A School-Aged Child is a 12 page guide created to assist speech language pathologists in the decision making process of how to select assessment instruments and prioritize assessment for school age children. The goal is to eliminate administration of unnecessary or irrelevant tests and focus on the administration of instruments directly targeting the areas of difficulty that the child presents with.
It contains:
Checklist Target Areas:
Auditory Processing Deficits Checklist for School Aged Children was created to assist speech language pathologists (SLPs) with figuring out whether the student presents with auditory processing deficits which require further follow up (e.g., screening, comprehensive assessment). The SLP should provide this form to both teacher and caregiver/s to fill out to ensure that the deficit areas are consistent across all settings and people.
Checklist Categories:
General Organizational Abilities
Social Pragmatic Deficits Checklist for School Aged Children was created to assist speech language pathologists (SLPs) with figuring out whether the student presents with social pragmatic language deficits which require further follow up (e.g., assessment). The SLP should provide this form to both teacher and caregiver/s to fill out to ensure that the deficit areas are consistent across all settings and people.
Checklist Categories:
You can find these products by clicking on the individual links above. You can also find many other educational products relevant to assessment and treatment in speech language pathology in my online store by clicking HERE.

Happy and successful new school year everyone!
 Recently I’ve purchased the Executive Functions Test-Elementary (EFT-E) by Linguisystems and used it with a few clients in my private practice and outpatient hospital-based school program. The EFT-E is a test of language skills that affect executive functions of working memory, problem solving, inferring, predicting outcomes, and shifting tasks. For those of you not familiar with executive functions (EFs), they are higher level cognitive processes involved in inhibition of thought, action and emotion, which are located in the prefrontal cortex of the frontal lobe of the brain. Continue reading The Executive Functions Test-Elementary (EFT-E): What SLPs and Parents Need to Know
Recently I’ve purchased the Executive Functions Test-Elementary (EFT-E) by Linguisystems and used it with a few clients in my private practice and outpatient hospital-based school program. The EFT-E is a test of language skills that affect executive functions of working memory, problem solving, inferring, predicting outcomes, and shifting tasks. For those of you not familiar with executive functions (EFs), they are higher level cognitive processes involved in inhibition of thought, action and emotion, which are located in the prefrontal cortex of the frontal lobe of the brain. Continue reading The Executive Functions Test-Elementary (EFT-E): What SLPs and Parents Need to Know
 In my social pragmatic language groups I target a wide variety of social communication goals for children with varying levels and degrees of impairment with a focus on improving their social pragmatic language competence. In the past I have written blog posts on a variety of social pragmatic language therapy topics, including strategies for improving students’ emotional intelligence as well as on how to teach students to develop insight into own strengths and weaknesses. Today I wanted to discuss the importance of teaching students with social communication impairments, age recognition for friendship and safety purposes.
In my social pragmatic language groups I target a wide variety of social communication goals for children with varying levels and degrees of impairment with a focus on improving their social pragmatic language competence. In the past I have written blog posts on a variety of social pragmatic language therapy topics, including strategies for improving students’ emotional intelligence as well as on how to teach students to develop insight into own strengths and weaknesses. Today I wanted to discuss the importance of teaching students with social communication impairments, age recognition for friendship and safety purposes.
Now it is important to note that the focus of my sessions is a bit different from the focus of “teaching protective behaviors”, “circles of intimacy and relationships” or “teaching kids to deal with tricky people“. Rather the goal is to teach the students to recognize who it is okay “to hang out” or be friends with, and who is considered to be too old/too young to be a friend.

Why is it important to teach age recognition?
There are actually quite a few reasons.
Firstly, it is a fairly well-known fact that in the absence of age-level peers with similar weaknesses, students with social communication deficits will seek out either much younger or much older children as playmates/friends as these individuals are far less likely to judge them for their perceived social deficits. While this may be a short-term solution to the “friendship problem” it also comes with its own host of challenges. By maintaining relationships with peers outside of their age group, it is difficult for children with social communication impairments to understand and relate to peers of their age group in school setting. This creates a wider chasm in the classroom and increases the risk of peer isolation and bullying.
Secondly, the difficulty presented by friendships significantly outside of one’s peer group, is the risk of, for lack of better words, ‘getting into trouble’. This may include but is not limited to exploring own sexuality (which is perfectly normal) with a significantly younger child (which can be problematic) or be instigated by an older child/adolescent in doing something inappropriate (e.g, shoplifting, drinking, smoking, exposing self to peers, etc.).
Thirdly, this difficulty (gauging people’s age) further exacerbates the students’ social communication deficits as it prevents them from effectively understanding such pragmatic parameters such as audience (e.g., with whom its appropriate to use certain language in a certain tone and with whom it is not) and topic (with whom it is appropriate to discuss certain subjects and with whom it is not).
![]()
So due to the above reasons I began working on age recognition with the students (6+ years of age) on my caseload diagnosed with social communication and language impairments. I mention language impairments because it is very important to understand that more and more research is coming out connecting language impairments with social communication deficits. Therefore it’s not just students on the autism spectrum or students with social pragmatic deficits (an official DSM-5 diagnosis) who have difficulties in the area of social communication. Students with language impairments could also benefit from services focused on improving their social communication skills.
I begin my therapy sessions on age recognition by presenting the students with photos of people of different ages and asking them to attempt to explain how old do they think the people in the pictures are and what visual clues and/or prior knowledge assisted them in the formulation of their responses. I typically select the pictures from some of the social pragmatic therapy materials packets that I had created over the years (e.g., Gauging Moods, Are You Being Social?, Multiple Interpretations, etc.).
I make sure to carefully choose my pictures based on the student’s age and experience to ensure that the student has at least some degree of success making guesses. So for a six-year-old I would select pictures of either toddlers or children his/her age to begin teaching them recognition of concepts: “same” and “younger” (e.g., Social Pragmatic Photo Bundle for Early Elementary Aged Children).
For older children, I vary the photos of different aged individuals significantly. I also introduce relevant vocabulary words as related to a particular age demographic, such as:
I explain to the students that people of different ages look differently and teach them how to identify relevant visual clues to assist them with making educated guesses about people’s ages. I also use photos of my own family or ask the students to bring in their own family photos to use for age determination of people in the presented pictures. When students learn the ages of their own family members, they have an easier time determining the age ranges of strangers.
My next step is to explain to students the importance of understanding people’s ages. I present to the students a picture of an individual significantly younger or older than them and ask them whether it’s appropriate to be that person’s friend. Here students with better developed insight will state that it is not appropriate to be that person’s friend because they have nothing in common with them and do not share their interests. In contrast, students with limited insight will state that it’s perfectly okay to be that person’s friend.
This is the perfect teachable moment for explaining the difference between “friend” and “friendly”. Here I again reiterate that people of different ages have significantly different interests as well as have significant differences in what they are allowed to do (e.g., a 16-year-old is allowed to have a driver’s permit in many US states as well as has a later curfew while an 11-year-old clearly doesn’t). I also explain that it’s perfectly okay to be friendly and polite with older or younger people in social situations (e.g., say hello all, talk, answer questions, etc.) but that does not constitute true friendship.
I also ask students to compile a list of qualities of what they look for in a “friend” as well as have them engage in some perspective taking (e.g, have them imagine that they showed up at a toddler’s house and asked to play with him/her, or that a teenager came into their house, and what their parents reaction would be?).
Finally, I discuss with students the importance of paying attention to who wants to hang out/be friends with them as well as vice versa (individuals they want to hang out with) in order to better develop their insight into the appropriateness of relationships. I instruct them to think critically when an older individual (e.g, young adult) wants to get particularly close to them. I use examples from an excellent post written by a colleague and good friend, Maria Del Duca of Communication Station Blog re: dealing with tricky people, in order to teach them to recognize signs of individuals crossing the boundary of being friendly, and what to do about it.
So there you have it. These are some of the reasons why I teach age recognition to clients with social communication weaknesses. Do you teach age recognition to your clients? If so, comment under this post, how do you do it and what materials do you use?
Helpful Smart Speech Resources Related to Assessment and Treatment of Social Pragmatic Disorders

 Today’s guest post on Williams Syndrome comes from Pamela Mandell, M.S. CCC-SLP with a contribution from Priya Deonarain, MA, OTR/L, CKTP.
Today’s guest post on Williams Syndrome comes from Pamela Mandell, M.S. CCC-SLP with a contribution from Priya Deonarain, MA, OTR/L, CKTP.
Overview
Williams syndrome (WS), also known as Williams-Beuren Syndrome, is a rare genetic disorder caused by the deletion of the long arm of chromosome 7 or, more specifically a microdeletion at 7q11.23, which involves the elastin gene. WS occurs in approximately 1 in 10,000 births worldwide. It is characterized by cardiovascular disease, dysmorphic craniofacial features, a characteristic cognitive and personality profile, deficient visuospatial abilities, hyperacusis, growth retardation, developmental delays, feeding difficulties, and learning disabilities. However, many people with WS exhibit strong expressive language skills and an affinity for music. Mild to severe anxieties as well as Attention Deficit Hyperactivity Disorder (ADHD) are also associated with WS. The degree of severity or involvement of these characteristics is variable and no two individuals with WS are alike. WS affects both males and females equally. Sadler, et al. (2001), determined the severity of both supravalvular aortic stenosis (SVAS) and total cardiovascular disease was significantly higher in males than females. There is no cure for WS. Patients must be continually monitored and treated for symptoms throughout their lives. Continue reading Spotlight on Syndromes: An SLPs and OTs Perspective on Williams Syndrome
 Here’s a familiar scenario to many SLPs. You’ve administered several standardized language tests to your student (e.g., CELF-5 & TILLS). You expected to see roughly similar scores across tests. Much to your surprise, you find that while your student attained somewhat average scores on one assessment, s/he had completely bombed the second assessment, and you have no idea why that happened.
Here’s a familiar scenario to many SLPs. You’ve administered several standardized language tests to your student (e.g., CELF-5 & TILLS). You expected to see roughly similar scores across tests. Much to your surprise, you find that while your student attained somewhat average scores on one assessment, s/he had completely bombed the second assessment, and you have no idea why that happened.
So you go on social media and start crowdsourcing for information from a variety of SLPs located in a variety of states and countries in order to figure out what has happened and what you should do about this. Of course, the problem in such situations is that while some responses will be spot on, many will be utterly inappropriate. Luckily, the answer lies much closer than you think, in the actual technical manual of the administered tests.
So what is responsible for such as drastic discrepancy? A few things actually. For starters, unless both tests were co-normed (used the same sample of test takers) be prepared to see disparate scores due to the ability levels of children in the normative groups of each test. Another important factor involved in the score discrepancy is how accurately does the test differentiate disordered children from typical functioning ones.
Let’s compare two actual language tests to learn more. For the purpose of this exercise let us select The Clinical Evaluation of Language Fundamentals-5 (CELF-5) and the Test of Integrated Language and Literacy (TILLS). The former is a very familiar entity to numerous SLPs, while the latter is just coming into its own, having been released in the market only several years ago.
Both tests share a number of similarities. Both were created to assess the language abilities of children and adolescents with suspected language disorders. Both assess aspects of language and literacy (albeit not to the same degree nor with the same level of thoroughness). Both can be used for language disorder classification purposes, or can they?
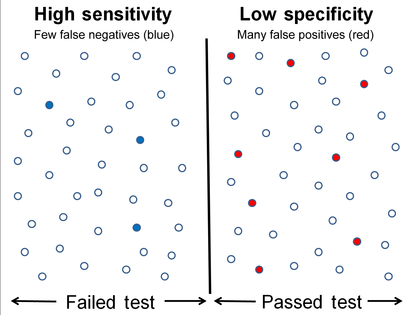 Actually, my last statement is rather debatable. A careful perusal of the CELF – 5 reveals that its normative sample of 3000 children included a whopping 23% of children with language-related disabilities. In fact, the folks from the Leaders Project did such an excellent and thorough job reviewing its psychometric properties rather than repeating that information, the readers can simply click here to review the limitations of the CELF – 5 straight on the Leaders Project website. Furthermore, even the CELF – 5 developers themselves have stated that: “Based on CELF-5 sensitivity and specificity values, the optimal cut score to achieve the best balance is -1.33 (standard score of 80). Using a standard score of 80 as a cut score yields sensitivity and specificity values of .97. “
Actually, my last statement is rather debatable. A careful perusal of the CELF – 5 reveals that its normative sample of 3000 children included a whopping 23% of children with language-related disabilities. In fact, the folks from the Leaders Project did such an excellent and thorough job reviewing its psychometric properties rather than repeating that information, the readers can simply click here to review the limitations of the CELF – 5 straight on the Leaders Project website. Furthermore, even the CELF – 5 developers themselves have stated that: “Based on CELF-5 sensitivity and specificity values, the optimal cut score to achieve the best balance is -1.33 (standard score of 80). Using a standard score of 80 as a cut score yields sensitivity and specificity values of .97. “
In other words, obtaining a standard score of 80 on the CELF – 5 indicates that a child presents with a language disorder. Of course, as many SLPs already know, the eligibility criteria in the schools requires language scores far below that in order for the student to qualify to receive language therapy services.
In fact, the test’s authors are fully aware of that and acknowledge that in the same document. “Keep in mind that students who have language deficits may not obtain scores that qualify him or her for placement based on the program’s criteria for eligibility. You’ll need to plan how to address the student’s needs within the framework established by your program.”
 But here is another issue – the CELF-5 sensitivity group included only a very small number of: “67 children ranging from 5;0 to 15;11”, whose only requirement was to score 1.5SDs < mean “on any standardized language test”. As the Leaders Project reviewers point out: “This means that the 67 children in the sensitivity group could all have had severe disabilities. They might have multiple disabilities in addition to severe language disorders including severe intellectual disabilities or Autism Spectrum Disorder making it easy for a language disorder test to identify this group as having language disorders with extremely high accuracy. ” (pgs. 7-8)
But here is another issue – the CELF-5 sensitivity group included only a very small number of: “67 children ranging from 5;0 to 15;11”, whose only requirement was to score 1.5SDs < mean “on any standardized language test”. As the Leaders Project reviewers point out: “This means that the 67 children in the sensitivity group could all have had severe disabilities. They might have multiple disabilities in addition to severe language disorders including severe intellectual disabilities or Autism Spectrum Disorder making it easy for a language disorder test to identify this group as having language disorders with extremely high accuracy. ” (pgs. 7-8)
Of course, this begs the question, why would anyone continue to administer any test to students, if its administration A. Does not guarantee disorder identification B. Will not make the student eligible for language therapy despite demonstrated need?
The problem is that even though SLPs are mandated to use a variety of quantitative clinical observations and procedures in order to reliably qualify students for services, standardized tests still carry more value then they should. Consequently, it is important for SLPs to select the right test to make their job easier.
 The TILLS is a far less known assessment than the CELF-5 yet in the few years it has been out on the market it really made its presence felt by being a solid assessment tool due to its valid and reliable psychometric properties. Again, the venerable Dr. Carol Westby had already done such an excellent job reviewing its psychometric properties that I will refer the readers to her review here, rather than repeating this information as it will not add anything new on this topic. The upshot of her review as follows: “The TILLS does not include children and adolescents with language/literacy impairments (LLIs) in the norming sample. Since the 1990s, nearly all language assessments have included children with LLIs in the norming sample. Doing so lowers overall scores, making it more difficult to use the assessment to identify students with LLIs. (pg. 11)”
The TILLS is a far less known assessment than the CELF-5 yet in the few years it has been out on the market it really made its presence felt by being a solid assessment tool due to its valid and reliable psychometric properties. Again, the venerable Dr. Carol Westby had already done such an excellent job reviewing its psychometric properties that I will refer the readers to her review here, rather than repeating this information as it will not add anything new on this topic. The upshot of her review as follows: “The TILLS does not include children and adolescents with language/literacy impairments (LLIs) in the norming sample. Since the 1990s, nearly all language assessments have included children with LLIs in the norming sample. Doing so lowers overall scores, making it more difficult to use the assessment to identify students with LLIs. (pg. 11)”
Now, here many proponents of inclusion of children with language disorders in the normative sample will make a variation of the following claim: “You CANNOT diagnose a language impairment if children with language impairment were not included in the normative sample of that assessment!” Here’s a major problem with such assertion. When a child is referred for a language assessment, we really have no way of knowing if this child has a language impairment until we actually finish testing them. We are in fact attempting to confirm or refute this fact, hopefully via the use of reliable and valid testing. However, if the normative sample includes many children with language and learning difficulties, this significantly affects the accuracy of our identification, since we are interested in comparing this child’s results to typically developing children and not the disordered ones, in order to learn if the child has a disorder in the first place. As per Peña, Spaulding and Plante (2006), “the inclusion of children with disabilities may be at odds with the goal of classification, typically the primary function of the speech pathologist’s assessment. In fact, by including such children in the normative sample, we may be “shooting ourselves in the foot” in terms of testing for the purpose of identifying disorders.”(p. 248)
 Then there’s a variation of this assertion, which I have seen in several Facebook groups: “Children with language disorders score at the low end of normal distribution“. Once again such assertion is incorrect since Spaulding, Plante & Farinella (2006) have actually shown that on average, these kids will score at least 1.28 SDs below the mean, which is not the low average range of normal distribution by any means. As per authors: “Specific data supporting the application of “low score” criteria for the identification of language impairment is not supported by the majority of current commercially available tests. However, alternate sources of data (sensitivity and specificity rates) that support accurate identification are available for a subset of the available tests.” (p. 61)
Then there’s a variation of this assertion, which I have seen in several Facebook groups: “Children with language disorders score at the low end of normal distribution“. Once again such assertion is incorrect since Spaulding, Plante & Farinella (2006) have actually shown that on average, these kids will score at least 1.28 SDs below the mean, which is not the low average range of normal distribution by any means. As per authors: “Specific data supporting the application of “low score” criteria for the identification of language impairment is not supported by the majority of current commercially available tests. However, alternate sources of data (sensitivity and specificity rates) that support accurate identification are available for a subset of the available tests.” (p. 61)
Now, let us get back to your child in question, who performed so differently on both of the administered tests. Given his clinically observed difficulties, you fully expected your testing to confirm it. But you are now more confused than before. Don’t be! Search the technical manual for information on the particular test’s sensitivity and specificity to look up the numbers. Vance and Plante (1994) put forth the following criteria for accurate identification of a disorder (discriminant accuracy): “90% should be considered good discriminant accuracy; 80% to 89% should be considered fair. Below 80%, misidentifications occur at unacceptably high rates” and leading to “serious social consequences” of misidentified children. (p. 21)
Review the sensitivity and specificity of your test/s, take a look at the normative samples, see if anything unusual jumps out at you, which leads you to believe that the administered test may have some issues with assessing what it purports to assess. Then, after supplementing your standardized testing results with good quality clinical data (e.g., narrative samples, dynamic assessment tasks, etc.), consider creating a solidly referenced purchasing pitch to your administration to invest in more valid and reliable standardized tests.
Hope you find this information helpful in your quest to better serve the clients on your caseload. If you are interested in learning more regarding evidence-based assessment practices as well as psychometric properties of various standardized speech-language tests visit the SLPs for Evidence-Based Practice group on Facebook learn more.
References:
 Today’s guest post on genetic syndromes comes from Lauren Laur, who is contributing a post on the 22q11.2 Deletion Syndrome.
Today’s guest post on genetic syndromes comes from Lauren Laur, who is contributing a post on the 22q11.2 Deletion Syndrome.
22q11.2 Deletion Syndrome is a syndrome of many names. Also known as Velocardiofacial Syndrome, Shprintzen syndrome as well as DiGeorge Syndrome, 22q11.2 Deletion Syndromeis is caused by a microdeletion on the long arm of chromosome 22 (at location marker q11.2). This syndrome follows an autosomal dominant inheritance pattern (a child only needs to get the abnormal gene from one parent in order to inherit the disease), however, only around 10% of cases are inherited; the majority of cases are due to a random mutation. Continue reading Spotlight on Syndromes: An SLPs Perspective on 22q Deletion Syndrome